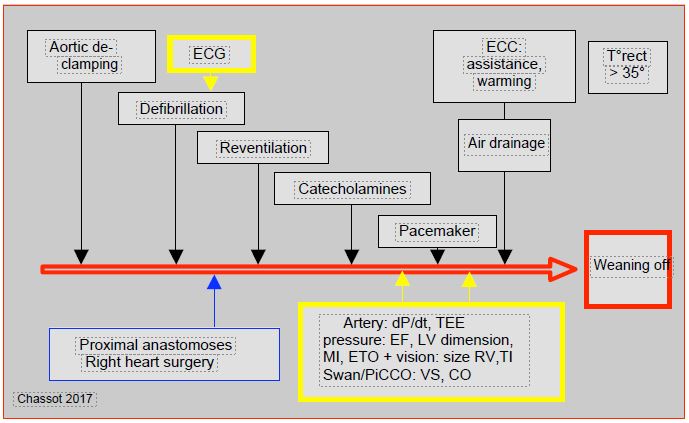
A number of conditions are required to wean the patient off bypass (Figure 7.45 and Table 7.7) [1].
Figure 7.45 Sequence of events and anaesthetic actions leading to weaning. The monitoring elements are highlighted in yellow and the surgical events in blue.
- Patient uniformly warmed; rectal T° should be ≥ 35°C, oesophageal temperature ≥ 36°C.
- Lungs re-expanded by vital capacity manoeuvres (manual insufflations at 30-40 cm H2 O for 20-30 seconds), taking care not to interfere the surgical field or distend the mammery graft [4].
- Effective ventilation; FiO2 is set to ensure SpO2 > 98%, monitored by blood gas analysis (PaO2 ≥ 100 mmHg); ScO2 (NIRS) is also an effective benchmark. Excessive FiO2 may worsen myocardial reperfusion injury. Ventilation is resumed when the heart is reperfused, i.e. after aortic decompression and resumption of spontaneous heart rhythm, or after revascularisation with coronary artery bypass grafts. Sometimes ventilation has to be interrupted because the lungs invade the surgical field and interfere with the surgeon activity.
- At the onset of rebreathing, airway pressure may be momentarily elevated and bronchoconstriction may lead to air trapping. This is related to lung collapse, atelectasis and the release of bronchoactive substances. It is important to reventilate early enough to ensure that this phenomenon is over by the time of weaning [2].
- Sleep with an intravenous agent (propofol, midazolam) and discontinue halogens if ventricular function is reduced. Even a low concentration of halogen can have adverse effects at the critical time of weaning. Halogen used in bypass surgery should be discontinued 10-15 minutes before weaning to ensure that its vasodilatory and negative inotropic effects have disappeared.
- Analgesia: addition of a dose of fentanil adapted for the case. Morphine 10mg at the end of the bypass provides analgesia for the early postoperative phase and minimises the risk of respiratory depression compared to an injection closer to recovery. For fast-track cases, sternal infiltration and intercostal blocks at closure are preferable. Dexmedetomidine (2-1.0 mcg/kg/hour) has both analgesic and sedative effects [5] and tends to become a routine measure at the end of the surgery.
- Sinus rhythm at 75-90 beats/min; cardioversion (10-20 joules) for atrial fibrillation. Iterative defibrillation (20-50 J) for recurrent episodes of ventricular fibrillation. Stabilisation of rhythm with amiodarone (Cordarone® 150 mg iv slow). Defibrillation may be required 10-20 times in a row for reperfusion injury, but recovery is complete in the long term (never give up!).
- Ventricular pacemaker leads in place and functional (pacemaker tested). Ventricular electrical pacing at 75 beats/min in case of AV block or bradycardia. If the rhythm is too slow, the LV does not eject blood to fill it from the bronchial circulation or aortic insufficiency in time; it may dilate dangerously. While waiting for the pacemaker, the operator can mechanically trigger regular ESVs with a metal instrument.
- MAP > 60 mmHg and < 120 mmHg; if not, address the haemodynamic problem first.
- PAP values corresponding to preoperative values or lower.
- Using the formula for calculating resistances, one can easily assess whether the patient is vasoconstricted or vasoplegic, since CVP is the ambient pressure (CVP = 0) and cardiac output is the pump output (PO = pump output). Therefore : RAS = (PAM - 80) / PO [3].
- PA curve on Swan-Ganz catheter tracing, deflated balloon; it is imperative never to inflate the catheter balloon without a clear pulmonary artery curve. Inflating the balloon while the catheter tip is in a blocked position would cause arterial rupture and massive pulmonary haemorrhage in a patient still receiving heparin.
- Adequate blood volume (volume in the bypass reservoir), degree of RV filling in the operating field.
- Adequate drainage of air that may have entered the left heart (TEE check).
- Control of kalaemia (< 6 mmol/L); a bolus of Ca2+ counteracts the effects of hyperkalaemia, but may induce arterial spasm, especially the mammery graft. Other means of lowering kalaemia: haemofiltration, insulin/glucose infusion, diuretic.
- Check acid-base balance, blood glucose (< 10 mmol/L) and Hb (> 60 g/L); treat as needed before weaning.
- Coagulation status: ACT, ROTEM™ (Fibtem, Heptem), possibly thrombocytes [6].
- TEE: effective debulking; right and left ventricular contractility, normal segmental kinetics for the case, volume of the chambers and possible valvular insufficiency corresponding to the images expected according to the pathology [3].
- Catecholamine and/or other selected inotropic agent administered centrally (or Swan-Ganz OD) 5-10 minutes before weaning.
- Reinstated infusions and functional venous lines.
- Alarms functional and volume restored; zero sensor checked.
- Blood bags, fibrinogen, clotting factors, thrombocytes are available as needed.
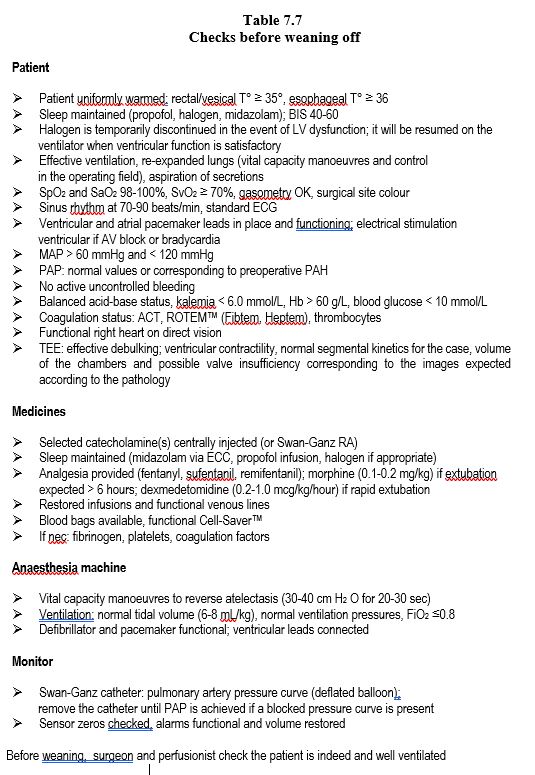
| Checks before weaning |
| Patient normothermic (T° rectal ≥ 35°, T° oeso ≥ 36°) and ventilated (FiO2 for SpO2 > 98% and PaO2 > 100 mmHg), lungs re-expanded
Sleep, analgesia and curarization provided
ECG satisfactory
Spontaneous cardiac activity, sinus rhythm or paced; defibrillation/cardioversion if necessary
Pace-maker (ventricular wires) in place and tested
Debulked left cavities
TEE: ventricular function, mitral/tricuspid insufficiency, segmental contractility, blood volume
Selected inotropic agent(s): running infusion
Removal of the Swan-Ganz catheter to obtain a PA curve before balloon inflation
MAP, PAP, SAR, SvO2 , Ht, lactate, electrolytes, blood glucose: within acceptable limits as appropriate
Pressure lines zeroed, alarms reset on monitor
|
© CHASSOT PG, GRONCHI F, April 2008, last update, December 2019
References
BARRY AE, CHANEY MA, LONDON MJ. Anaesthetic management during cardiopulmonary bypass: a systematic review. Anesth Analg 2015; 120:749-69
BAUFRETON C, MOREAU X, CORBEAU JJ, et al. Standard ECC and new consumable devices. In: JANVIER G, LEHOT JJ (ed). Circulation extracorporelle: principes et pratique, 2nd edition. Paris, Arnette Groupe Liaison SA, 2004, pp 113-45
DENAULT AY, BUSSIERES J, CARRIER M, et al. The importance of difficult separation from cardiopulmonary bypass: the Montreal and Quebec Heart Institute experience. Exp Clin Cardiol 2006; 11:37
MAGNUSSON L, ZEMGULIS V, RENLING A, et al. Use of a vital capacity maneuver to prevent atelectasis after cardiopulmonary bypass. Anesthesiology 1998; 88:134-42
SCHNABEL A, MEYER-FRIEBEM C, REICHL S, et al. Is intraoperative dexmedetomidine a new option for postoperative pain treatment? A meta-analysis of randomized controlled trials. Pain 2013; 154: 1140-9
WEBER CF, GÖRLINGER K, MEININGER D. Point-of-care testing: a prospective randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology 2012; 117: 531-47
© CHASSOT PG, GRONCHI F, April 2008, last update, December 2019