By analogy with heart failure, the clinical course of valvular heart disease can be divided into four stages [6].
- A: Risk situations; asymptomatic patients with simple risk factors.
- B: Progressive valve disease; asymptomatic patients with mild or moderate valve pathology.
- C: severe but asymptomatic valve disease; criteria for severity present on echocardiography, angio-CT or catheterisation.
- C1: LV and RV function still compensated.
- C2: left and/or right ventricular decompensation.
- D: Severe and symptomatic valvulopathy.
While the indication for surgery is easy to establish when patients are symptomatic or meet the criteria for severe valvulopathy (see definitions for each valve), it is more difficult to decide to operate on an asymptomatic or paucisymptomatic patient. In these circumstances, a number of criteria come into play.
- Echocardiographic monitoring can detect when the dimensions of the ventricle or atrium change significantly. Beyond the upper normal limits (DtsLV > 2.5 cm/m2 , DtdLV > 4.0 cm/m2 , DRA > 5.0 cm), valve correction is recommended even in paucisymptomatic patients [1]. However, these criteria have been shown to be inappropriate for women with valvular regurgitation, as they become symptomatic before these degrees of dilatation are reached [5].
- A reduction in systolic performance or the onset of arrhythmia (AF) also determines the time to intervene [1,4,6].
- Exercise testing can be used to identify patients who are asymptomatic because of spontaneous activity limitation but who are unable to exercise without an excessive increase in pressure gradient or systolic PAP [7,8].
- Although an independent risk factor for valve surgery, age (> 75 years) is no longer a contraindication to surgery, especially for aortic stenosis [3,9,10].
- The trend towards reconstructive surgery rather than valve replacement and the improved surgical outcomes of these reconstructions have led to the indication for surgery being given earlier in the course of the disease and therefore to patients being operated on in a better clinical condition.
In general, echocardiography has become sufficiently effective to provide all the data needed to make an indication for surgery. Exercise testing can be used to stratify individual risk in asymptomatic patients whose reduced physical activity masks the reality of the disease (see Exercise testing). Catheterisation is now performed only in doubtful cases (< 5%), and coronary angiography in patients with ischaemic symptoms or over the age of 45 if valve replacement by bypass surgery is planned.
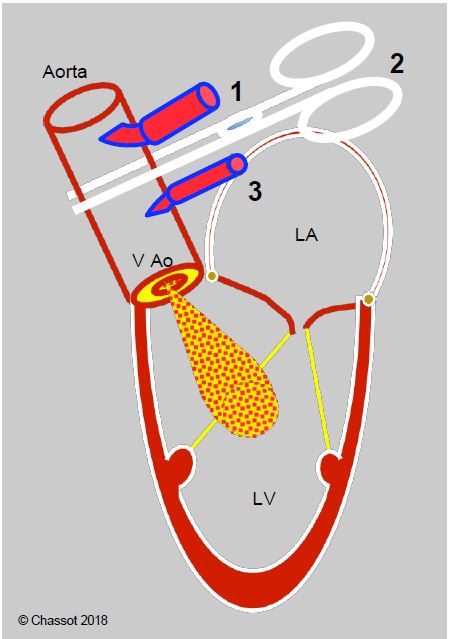
Any aortic insufficiency, however mild, carries a risk of ventricular dilatation during aortic root cardioplegia at the start of ECC because the heart stops beating efficiently and no longer ejects the volume it receives (Figure 11.33). The size of the ventricular cavity should be carefully monitored on TEE and, if the pressure is low, the temptation to inject vasoconstrictors, which would increase the aortic leak, should be avoided. Any increase in the size of the LV must be massaged and drained to empty it.
Figure 11.33: Diagram illustrating the risk of LV dilatation in AI at the start of ECC and during cardioplegia. At the start of ECC, the arterial cannula (1) delivers into the ascending aorta; as the LV gradually stops ejecting, there is a risk that it will fill with AI until the aortic clamp (2) blocks flow to the leaking valve. Cardioplegia solution (3) is delivered into the root of the aorta to perfuse the coronary arteries; in the event of AI, some of the solution will leak into the LV and there is a risk that it will dilate as it stops contracting.
| Indication for surgery |
| Generally speaking, valvulopathy is indicated for surgery in the following situations:
- Severe symptomatic valve disease - Severe asymptomatic valve disease with worsening ventricular damage - Moderate-to-severe or severe asymptomatic valve disease during cardiac surgery for another pathology - Refractory and/or embolising endocarditis |
References
- BAUMGARTNER H, FALK V, BAX JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017; 38:2739-86
- BONOW RO, BRAUNWALD E. Valvular heart disease. In: ZIPES DP, et al, eds. Braunwald's heart disease. A textbook of cardiovascular medicine. 7th edition. Philadelphia: Elsevier Saunders, 2005, 1553-632
- FILSOUFI F, RAHMANIAN PB, CASTILLO JG, et al. Excellent early and late outcomes of aortic valve replacement in people aged 80 and older. J Am Geriatr Soc 2008; 56:255-61
- IUNG B, GOHLKE-BÄRWOLF C, TORNOS P, et al. Recommendations on the management of the asymptomatic patient with valvular heart disease. Eur Heart J 2002; 23:1253-66
- KLODAS E, ENRIQUEZ-SARANO M, TAJIK AJ, et al. Surgery for aortic regurgitation in women: Contrasting indications and outcomes ompared with men. Circulation 1996; 94:2472-8
- NISHIMURA RA, OTTO CM, BONOW RO, et al. 2014 AHA/ACC Guideline for the management of patients with valvular heart disease. Circulation 2014; 129:e521-e643
- PICANO E, PIBAROT P, LANCELLOTTI P, et al. The emerging role of exercise testing and stress echocardiography in valvular heart disease. J Am Coll Cardiol 2009; 54:2251-60
- PIERARD LA, LANCELLOTTI P. Stress testing in valve disease. Heart 2007; 93:766-72
- SPEZIALE G, NASSO G, BARATTONI MC, et al. Operative and middle-term results of cardiac surgery in nonagenarians. A bridge toward routine practice. Circulation 2010; 121:208-13
- ZINGONE B, GATTI, RAUBER E, et al. Early and late outcomes of cardiac surgery in octogenarians. Ann Thorac Surg 2009; 87:71-8