Introduction
Isolated limb perfusion (ILP) allows the administration of large quantities of antimitotics while reducing the systemic toxicity of these substances. This technique also allows the limb to be maintained in hyperthermia (around 40°C), which increases the cytolytic efficacy of the agents. It is intended for patients with in-transit metastases of melanoma or sarcoma, isolated to a limb, without systemic dissemination. The survival of these patients is usually less than 6 months, even after disarticulation of the limb. Treatment allows limb salvage in 80% of cases, with an average survival of 3 to 5 years [3].
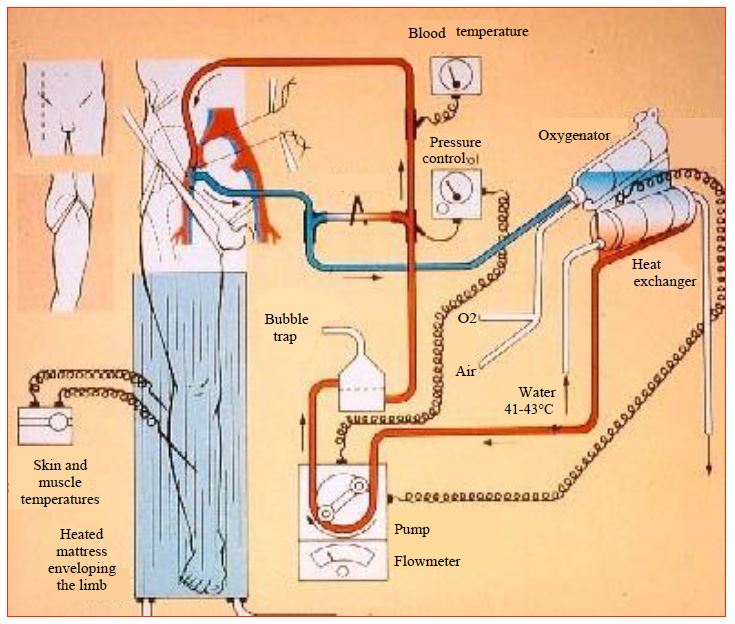
The bypass machine is connected to the iliac or femoral vessels (respectively axillary for the upper limb) and consists of pump, oxygenator and reservoir like a standard bypass machine, it supplies the limb isolated from the general body circulation (Figure 7.59).
Figure 7.59: Extracorporeal circulation system for isolated lower limb perfusion [203].
The substances used in ILP vary according to the indications.
- For melanoma: TNFa + Interferon-gamma (IFN) + melphalan;
- For very distal melanomas in elderly patients: melphalan alone;
- For sarcoma: TNFa + melphalan.
Systemic leakage from the isolated limb is unavoidable, but its magnitude depends on the relative overpressure created in the limb by the flow of the bypass machine; it is of little significance when the flow is maintained at 45 mL/min per litre of limb volume. These leaks result in side effects which intensity is proportional to their size and to the systemic toxicity of the substance used, the most damaging being TNF.
- Fluid exchange between the patient and the ECC;
- Systemic hyperthermia;
- Distributive shock due to massive vasoplegia, usually comes with pulmonary hypertension;
- Capillary Leak Syndrome;
- ARDS (occurs between 6 and 24 hours post-op);
- Hematological changes due to chemotherapy;
- Organ dysfunctions (renal, liver failure) due to TNF.
Anaesthesia technique
The technique is similar to that used in cardiac surgery but the patient is usually put to sleep before being fitted, unless associated with heart disease. Monitoring and management differ depending on whether the infusion contains TNF or not, as the risk of distributive shock and its intensity are very different in the two situations.
- Monitoring includes a radial arterial catheter (very possibly contralateral femoral) and a Swan-Ganz pulmonary catheter for cases with TNF infusion, or an arterial catheter and a central venous line for cases with melphalan alone; large bore venous lines.
- Prophylactic antibiotic therapy.
- Induction: propofol or etomidate depending on cardiovascular status.
- Anaesthetic input: propofol or sevoflurane, fentanyl or sufentanil.
- Starting the bypass graft; the pump rate is 45 mL/min per litre of limb volume (measured preoperatively). Fluid exchanges between the bypass machine and the patient are frequent during this phase, requiring the patient to be refilled or vasodilated on demand; the perfusionist can moderate these variations by adjusting the level of his venous reservoir. The priming fluid contains 200 mL of lactated Ringer's, 200 mL of colloid and 50 mg of heparin.
- Limb heating to 40°C (20-45 min) with the patient on the 42°C circulating water mattress and the limb covered by the 42°C Bair-Hugger™ mattress . Temperatures monitored are: distal skin, distal muscle, proximal skin, proximal muscle, ECC arterial line, rectum, oesophagus, pulmonary artery blood in case of Swan-Ganz. By the time a threshold temperature of 38°C is reached, the bypass is started.
- Injection of technecium labelled serum albumin systemically (10 mCi) and into the ECC (4 mCi). After equilibration (10-15 min), the precordial camera estimates leakage from the limb to the systemic circulation; a stable plateau in the isotope count, proving that leakage is less than 1%, must be achieved before TNF can be injected.
- Injection into the ECC reservoir of the substances according to the chosen protocol: TNF and or melphalan. Circulation for 60 minutes (melphalan) or 90 minutes (TNF).
- At the end of the pump, replace and flush the bypass volume with 2000 mL of empty Rheomacrodex-saline® and Ringer's lactate (up to 6000 mL when infusing with TNF); wash the limb by exsanguination until the flush fluid is clear.
- End of bypass; decanulation, protamine according to ACT, vascular reconstruction and patient recovery.
Hemodynamic problems
The surgical procedure carries a significant bleeding risk, requiring blood transfusions in most cases. During bypass surgery, fluid exchanges take place between the perfused limb and the systemic circulation, resulting in overloads or spoliations of the patient circulation. On the other hand, the inherent toxicity of the substances used causes a state of distributive shock namely a massive systemic inflammatory syndrome (SIRS), significant interstitial fluid extravasation (Capillary Leak Syndrome) and a severe decrease in systemic resistance leading to arterial hypotension (distributive shock). Usually comes with pulmonary hypertension and high cardiac output. The release of the tourniquet at the end of the bypass is the time of greatest haemodynamic disturbance, even in cases without TNF. However, it is clear that TNF is the main contributor to the haemodynamic effects, as the extent of distributive shock is proportional to circulating TNF levels, systemic resistances are much lower in cases with TNF than during simple tourniquet release (tourniquet effect), and cardiac output is significantly higher [1]. Flushing the limb also contributes to blood spoliation. Although TNF levels recorded may have been 10,000 times higher than those seen in lethal septic shock, all episodes of distributive shock, regardless of size, proved fully reversible [2].
Sustained tachycardia is often the first symptom of distributive shock. Vasodilation usually occurs late in the procedure, after bypass surgery; it may set in very abruptly. Administration of alpha stimulants (bolus phenylephrine, norepinephrine infusion) should be started early. Forced diuresis is recommended for several hours (Vu > 1 mL/kg/hour). Multifocal VSE may be induced by TNF and/or hypokalaemia and responds to lidocaine.
Treatment depends on the intensity of the symptoms.
- Filling: crystalloids and colloids, blood (maintain Hb > 80 g/L); requirements can be considerable (4-10 litres).
- Noradrenaline: infusion 2-5 mcg/min or more, to be titrated according to RAS; maintain MAP of 70-80 mm Hg for a normotensive patient.
- Dobutamine: 3-15 mcg/kg/min if ventricular failure; maintain cardiac index > 3.0 L/min/m2 .
- Maintain urine output above 1mL/kg/hour (infusions, mannitol, possibly furosemide if normovolaemia).
Post-operative care
The postoperative course is straightforward if there has been no significant release of substance. However, it has been demonstrated that, despite extensive lavage, recirculation of TNF occurs in most cases. There is a febrile state and a moderate hyperdynamic circulatory state with increased fluid requirements. When release is significant, the course is characterised by the persistence or onset within the first 12 hours of distributive shock, generalised increased capillary permeability and ARDS. Patients may also develop renal failure, DIC and superinfections (decreased immune resistance) [3]. These symptoms only occur with TNF administration. The infused limb should be carefully monitored because of compartment syndrome, ischaemia or vascular thrombosis.
| Isolated limb infusion |
|
Reduced-volume bypass surgery allows a limb to be perfused in a closed circuit with high concentrations of antimitotic drugs (TNF-a , melphalan) and warmed to 38-40°C. Indications: melanoma and sarcoma invading a limb but without distant metastases.
Despite clamps and isolation of the limb, systemic leakage occurs, resulting in the need for a more effective treatment:
- Massive vasoplegia (first sign: refractory tachycardia)
- Massive inflammatory syndrome
- Respiratory distress syndrome (capillary leak syndrome)
The haemodynamic effects are maximal at tourniquet release.
|
© CHASSOT PG, GRONCHI F, April 2008, last update, December 2019
References
- Christoforidis D, Chassot PG, Mosimann F, et al: Isolated limb perfusion: distinct tourniquet and tumor necrosis factor effects on the early hemodynamic response. Arch Surg 2003; 138:17-25
- Eggimann P, Chiolero R, Chassot PG, et al: Systemic and hemodynamic effects of recombinant tumor necrosis factor alpha in isolation perfusion of the limbs. Chest 1995; 107:1074-82
- Lejeune FJ, Kroon BB, Di Filippo F, et al: Isolated limb perfusion: the European experience. Surg Oncol Clin N Am 2001; 10:821-32