In clinical practice, precise knowledge of the anatomy of congenital heart disease is essential for understanding how it functions. Several examination methods are available (Table 15.2) [1,2,5,6].
- Echocardiography: this is an essential tool as it is the simplest, fastest, and most widely available technique. It provides information on basic anatomy and on the morphology of the heart chambers and valves and their function. The Doppler measures blood flows, gradients, shunts and, indirectly, RV and/or PA pressure (see Chapter 27 Congenital heart diseases). Transthoracic echocardiography (TTE) may be supplemented by transesophageal echocardiography (TEE) in order to achieve greater precision when viewing delicate or posterior structures (endocarditis, pulmonary veins, ASD, mitral valve). Echocardiography is well suited to functional assessments of the LV due to its relatively simple shape. However, it is less effective for assessing the RV due to its complex morphology, even when special techniques are used, such as measuring the tricuspid annular plane systolic excursion (TAPSE) or local deformation (strain and strain rate) [4,7]. With the exception of TEE for the descending aorta (coarctation), it is not appropriate for examining extra-cardiac vessels. 3D echocardiography offers greater accuracy, especially when assessing atrioventricular valves, septa (ASD, VSD, AV canal defect) and the RV. However, compared to MRI, 3D echocardiography tends to underestimate RV volume [3].
- MRI: provides a very detailed three-dimensional reconstruction of the anatomy and is superior to an echocardiogram in terms of assessing the RV, chamber volume, tissue characteristics (viability) and extra-cardiac vessels (pulmonary veins, aorta, PA, collaterals). It can also be used to measure flows and calculate shunts, gradients or the regurgitation fraction of valve insufficiencies. However, it requires 10-20 second periods of apnoea to acquire images, a regular heart rate, and a lack of metal devices such as pacemakers and prostheses [9]. Calcification causes artefacts.
- CT-scan: multislice CT scans are more widely available and faster than MRI, offering superior anatomical definition of structures, particularly those that are extra-cardiac. However, its drawback is the use of ionising radiation and contrast agents. It is used to screen for coronary artery lesions, but requires a relatively low heart rate. It clearly reveals calcifications and bony structures.
- Angiocatheterisation: this is used solely to define extra-cardiac vessels and accurately measure right-sided pressure (PAP, PVR) or pulmonary vascular reactivity (NO test). Angiography is currently only indicated for assessing the coronary arteries (ischaemic patients) and aortopulmonary collateral arteries.
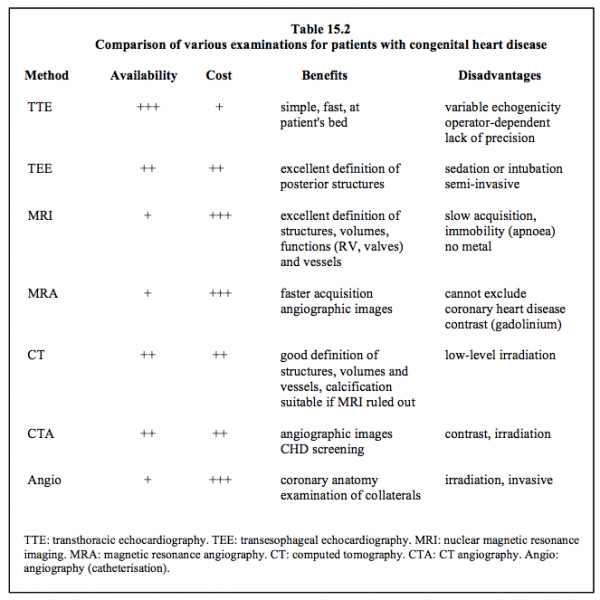
Generally, MRI and CT-scans are only used in situations that cannot be clarified with echocardiography. They offer the benefit of providing multiple viewing angles and not being dependent on an examination window.
| Diagnostic examinations |
| Several cardiological examinations are available for honing diagnosis: - Echocardiography (TTE, TEE): simple, fast, widely available - MRI: better definition of structures, volumes and the RV - CT-scan: if MRI not possible - Angiography: only indicated for coronary arteriography and detecting aorta-PA collaterals - Catheterisation: accurate measurement of PAP and PVR, NO test |
© BETTEX D, CHASSOT PG, January 2008, last update February 2020
References
- BAUMGARTNER H, BONHOEFFER P, DE GROOT NMS, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 2010; 31:2915-57
- BHATT AB, FOSTER E, KUEHL K, et al. Congenital hesart disease in older adult. A Scientific Statement from the American Heart Association. Circulation 2015; 131:1884-931
- CREAN AM, MAREDIA N, BALLARD G, et al. 3D echo systematically underestimates right ventricular volumes compared to cardiovascular magnetic resonance in adult congenital heart disease patients with moderate or severe right ventricular dilatation. J Cardiovasc Magn Resn 2011; 13:78
- DAVLOUROS PA, NIWA K, WEBB G, GATZOULIS MA. The right ventricle in congenital heart disease. Heart 2006; 92(Suppl 1):i27-i38
- HO VB. Radiologic evaluation of suspected congenital heart disease in adults. Am Fam Physician 2009; 80:597-602
- STOUT KK, DANIELS CJ, VALENTE AM, et al. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease. J Am Coll Cardiol 2019; 73:e81-192
- VILLAFAÑE J, FEINSTEIN JA, JENKINS KJ, et al. Hot topics in tetralogy of Fallot. J Am Coll Cardiol 2013; 62:2155-66
