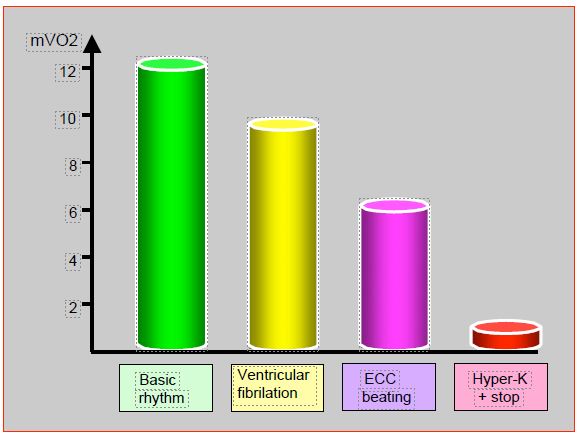
Oxygen consumption of the heart contracting at its baseline rate is 10-15 mL/100 gm/min; when in fibrillation, it drops to 8 mL/100 gm/min (75% of baseline consumption); when beating without producing ejection work during bypass surgery, the heart consumes only 50% of what it normally uses [2]. Diastolic arrest by potassium reduces O2 consumption to about 1 mL/100 gm/min in normothermia, and to 0.3 mL/100 gm/min in hypothermia. Thus the arrested heart has some oxygen requirement (Figure 7.55).
Figure 7.55: Cardiac oxygen consumption (mVO2 in mL/100gm/min) in different situations [2]. Basic rhythm: normal flow in sinus rhythm. Fibrill ventricul: average consumption in venricular fibrillation. Beating on bypass: spontaneous rhythm in full discharge, with circulation provided by bypass. Hyper-K + arrest: arrest in diastole by potassium rich cardioplegia.
The cardioplegia solution must stop the heart, protect it, and provide it with the elements for its survival until it resumes its activity. It must prevent the formation of free radicals and calcium overload. It is based on two elements [1].
- Hyperkalaemia stops the heart in diastole. The concentrations of K+ used in cardioplegia solutions vary between 18-20 mmol/L and 20-25 mmol/L for cold and warm solutions, respectively.
- Hypothermia is a major element in myocardial protection. The temperature is 5-10° for cold cardioplegia solutions.
As the heart continues to consume some energy by anaerobic glycolysis, the intracellular acidosis is buffered with Na-bicarbonate, trometamol (Tris or THAM), or other agents (histidine, acetate, phosphate). The addition of bicarbonate to cold solutions is a nonsense since the latter loses its buffering capacity in cold conditions; only the imidazole function of the histidine of the proteins retains the same degree of dissociation whatever the temperature, thus retaining its buffering capacity in deep hypothermia. This is one of the advantages of blood cardioplegia.
Several routes of administration are possible for the solution to reach the myocardium. A combined approach is therefore often necessary.
- Cannula in the aortic root; this is the classic route. It does not provide adequate perfusion in aortic insufficiency (AI); even minimal AI can lead to leakage into the LV and acute dilation of the ventricle. Perfusion pressure: 70-150 mmHg.
- Direct coronary cannulation with Spencer cannulas; used in cases of major AI or dissection, it carries the risk of distal atheromatous plaque embolisation when the cannula penetrates the coronary ostium. Perfusion pressure: 70-150 mmHg.
- Retrograde cardioplegia through the coronary sinus; it has the advantage of reaching distal territories in case of proximal tight stenoses with little collateralization and of avoiding aortic leakage, but it does not protect the right ventricle whose drainage is done by the veins of Thebesius and not by the coronary sinus. The cannula is inserted by puncturing the RA; it has a semi-occlusive balloon. The perfusion pressure must remain between 30 and 40 mmHg and is measured by a separate pressure transducer. The flow rate is 100-200 mL/min.
- Perfusion of the venous grafts as soon as the distal anastomosis is performed.
| Cardioplegia solutions |
| Cardioplegia should arrest the heart, protect it during the absence of perfusion, limit ischaemic injury and prevent reperfusion injury. The heart is stopped in diastole by a hyperkalaemic (K+ 18-25 mmol/L) and hypothermic (5-10°C) solution, to which various substances can be added. The solution may be crystalloid or based on blood from bypass. Infusion rate: 300 mL/min for arrest, 150 mL/min for maintenance.
Four approaches are possible: the root of the aorta (classical route), the coronary trunks (direct cannulation), the coronary sinus (retrograde route) or the venous grafts (after distal anastomosis).
|
© CHASSOT PG, GRONCHI F, April 2008, last update, December 2019
References
- RINNE TT. Cardioprotection and cardioplegia. In: THYS DM, et al, eds. Textbook of cardiothoracic anesthesiology. New York, McGraw-Hill Co, 2001, 488-511
- ROSENKRANZ ER. Myocardial preservation. In: ESTEFANOUS F, et al, Eds. Cardiac anesthesia. principles and clinical practice. Philadelphia, Lippincott Williams & Wilkins, 2001, 387-414