- Staphylococci 42%
- Streptococci 29%.
- Enterococci 10%
- HACEK group* 2%
- Fungi, yeasts 2%
- Negative blood cultures 10-20
- Staphylococci: flucloxacillin or penicillin are effective if the organisms are susceptible; gentamicin reduces the duration of bacteraemia. Vancomycin is recommended for MRSA; daptomycin is effective in cases of hyper-resistance.
- Streptococci: Betalactam monotherapy is the preferred treatment; in cases of intermediate resistance, an aminoglycoside is combined (monitor renal function).
- Enterococci: these organisms may be resistant to betalactams, aminoglycosides and vancomycin alone; in this case, the combination of ampicillin + ceftriaxone may be effective. Daptomycin may be a solution.
In 48% of cases of endocarditis, treatment leads to surgery to resect the infected structure, repair the valvular insufficiency or fistula, control the infection and prevent embolism. The degree of failure is such that surgery is often performed as an emergency within 48 hours after haemodynamic restoration and antibiotic coverage; once the indication has been established, delay is detrimental, except in the case of stroke (risk of intracranial haemorrhage) [2]. Indications for surgery are divided into three categories [1,4].
- Haemodynamic decompensation.
- Severe mitral or aortic regurgitation (often acute).
- Severe valve obstruction (obstructed winglets).
- Fistula resulting in cardiogenic shock.
- Uncontrolled infection.
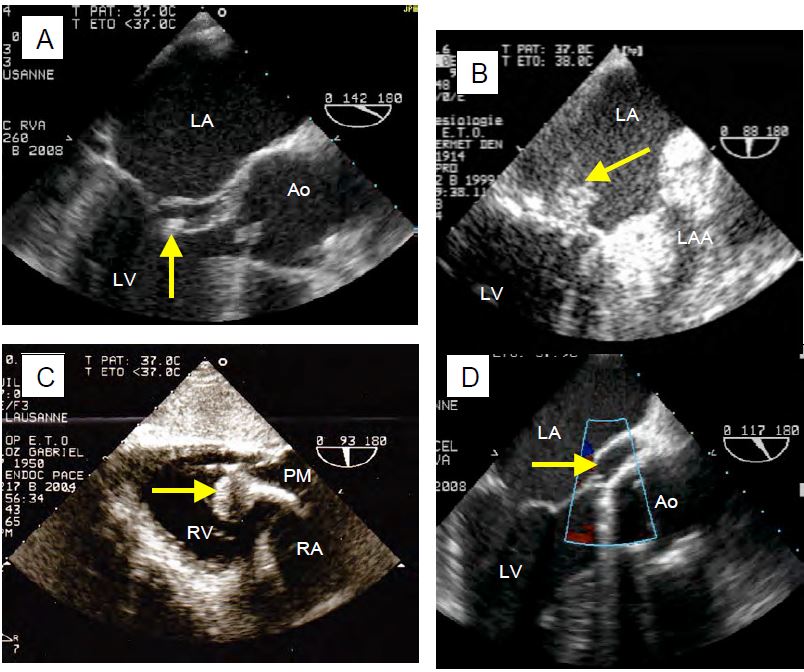
- Abscess, pseudoaneurysm (increasing in volume), complete AV block.
- Vegetation.
- Infection of prosthetic devices (mechanical valve, bioprosthesis, Dacron tube).
- Persistence of infection despite antibiotic treatment (fever, positive blood cultures).
- Prevention of emboli
- Aortic or mitral mobile vegetation > 10 mm with embolic event, abscess or cardiac decompensation.
- Aortic or mitral mobile vegetation > 15 mm.
- Tricuspid vegetation > 20 mm.
Valve repair is always preferable to prosthesis replacement in this setting, but is not always possible given the degree of valve destruction and extent of the lesion. If aortic reconstruction is required, a homograft is preferred. If the valve is infected, removal of the implanted device (pacemaker, catheter, etc) is recommended [7]. In-hospital mortality is 17%; 10-year survival is 40-60%, much lower than for elective valve surgery on a clean valve [6].
Prophylactic treatment
High velocity jets and the presence of prosthetic material are a cause of endothelial lesions leading to platelet and fibrin deposition; in the presence of bacteraemia, organisms can easily colonise these lesions and develop a focus of endocarditis [7]. This phenomenon is a high-risk situation requiring antibiotic prophylaxis in the event of surgery that could lead to bacteraemia [2,7,8].
- Presence of prosthetic material; the risk of endocarditis is highest with mechanical prostheses and foreign components (rings, tubes, patches, implanted material); it is lowest with bioprostheses; it is lowest with homografts. Endoprostheses such as TAVI carry the same risk as other prostheses. The presence of high velocity blood flow is an additional risk factor.
- Cyanotic congenital heart disease.
- Congenital heart disease with prosthetic material during the first 6 months after implantation or for life in the presence of high-velocity shunt/regurgitation.
- Heart transplant recipients with valvular insufficiency due to structural damage.
- History of endocarditis.
Low-velocity non-cyanogenic heart disease (ASD, PFO, coarctation), low mechanical stress valve disease (Barlow's disease, ischaemic or functional MI, dynamic subaortic obstruction) and functional insufficiencies are low-risk lesions that do not require prophylaxis, except where justified by the surgical procedure [1,4].
Although antibiotic prophylaxis is necessary in high-risk cases, recent recommendations favour a more balanced attitude between the risks associated with antibiotics, which are significant, and the benefits of prophylaxis, which are not very significant [1,4]. Prophylaxis is therefore no longer systematically recommended for all operations, unless it is part of the surgical procedure itself. A few comments are in order [7].
- Antibiotic prophylaxis for dental surgery is only justified in cases of gingival effraction, perforation of the mucosa, periapical surgery or dental abscess.
- Genitourinary or digestive endoscopic procedures (cystoscopy, gastroscopy, TEE, colonoscopy, etc.) do not require prophylaxis in the absence of active infection.
- With the exception of tonsillectomy, prophylaxis is no longer recommended for operations on the respiratory tract in the absence of active infection.
- Prophylaxis is no longer recommended in aortic stenosis, mitral stenosis, bicuspid aortic valve without haemodynamic consequences, coarctation of the aorta, mitral valve prolapse, functional insufficiency or obstructive cardiomyopathy, unless routine treatment is justified by the operation itself.
| Endocarditis prophylaxis |
|
Indications:
- Presence of prosthetic material
- Valvulopathy with high mechanical stress or associated with tissue degeneration
- Cyanotic or high velocity congenital heart disease
- History of endocarditis
Prophylaxis is no longer recommended in simple aortic or mitral stenosis, bicuspid aortic valve without haemodynamic consequences, mitral valve prolapse, functional insufficiency or obstructive cardiomyopathy, unless justified by the operation itself.
Indications for valve surgery (in addition to ongoing medical management)
- Ventricular failure in MI or AI
- AV block, aortic abscess, fistula, perforation
- Non-regression of lesions
- Embolization of vegetations > 10 mm
Specific surgical indications for prosthetic valve endocarditis: dehiscence, paravalvular leak, fin blockage, persistent bacteraemia.
|
References
- BADDOUR LM, WILSON WR, BAYER AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications. A Scientific Statement for healthcare professionals from the AHA. Circulation 2015; 132:1435-86
- CAHILL TJ, BADDOUR LM, HABIB G, et al. Challenges in infective endocarditis. J Am Coll Cardiol 2017; 69:325-44
- CAHILL TJ, PRENDERGAST BD. Infective endocarditis. Lancet 2016; 387:882-93
- HABIB G, LANCELLOTTI P, ANTUNES MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur Heart J 2015; 36:3075-123
- LI JS, SEXTON DJ, MICK N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000;30:633-8
- MANNE MB, SHRESTHA NK, LYTLE BW, et al. Outcomes after surgical treatment of native and prosthetic valve infective endocarditis. Ann Thorac Surg 2012; 93:489-93
- NISHIMURA RA, OTTO CM, BONOW RO, et al. 2014 AHA/ACC Guideline for the management of patients with valvular heart disease. Circulation 2014; 129:e521-e643
- NISHIMURA RA, OTTO CM, BONOW RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC Guideline for the management of patients with valvular heart disease. J Am Coll Cardiol 2017; 70:252-89
- ROSSEL A, CARBALLO D, CARBALLO S. Diagnosis and early management of infective endocarditis. Rev Méd Suisse 2012; 8:1966-71
- SONDEREGGER B, FÜHRER U, PORTMANN S, ZIMMERLI S. Infective endocarditis - Update part 1. Forum Med Suisse 2012; 12:608-12
- SONDEREGGER B, FÜHRER U, PORTMANN S, ZIMMERLI S. Infective endocarditis - Update part 2. Forum Med Suisse 2012; 12:624-
