Irrespective of each pathology’s idiosyncrasies, adult congenital heart disease patients experience many of the same problems and exhibit significant differences in comparison to children [1,3,4,5,6,7,9,11,12].
- Risk factors, which are as follows by order of seriousness:
- Pulmonary hypertension (mean PAP > 35 mmHg at rest);
- Cyanosis (SaO2 ≤ 85%);
- Reoperation, sequelae;
- Arrhythmias:
- Ventricular dysfunction;
- Anatomically right systemic ventricle;
- Severe obstruction of the ejection pathway.
- Mean surgical mortality of 5%, which is higher than the rate for children with related pathologies (cardiac surgery).
- A very high incidence of arrhythmias: 58% versus 15% in children.
- Ventricular remodelling causing dysfunction of the RV, LV, or both. Ventricular failure is linked to the pathology, duration of disease progression, and the presence of cyanosis.
- A pulmonary circulation anomaly: hypertension (PAH) or low blood flow (cyanosis).
- Systemic effects due to the long-term effects of hypoxia, hyperviscosity or venous stasis: renal, neurological, pulmonary, haematological, hepatic. These effects may result in severe postoperative decompensation secondary to even minor changes to perfusion conditions.
- Changes to coagulation.
- Comorbidity with age-related cardiovascular diseases: diabetes, coronary heart disease, arterial hypertension, bronchopathy.
Decisions over patient operability are taken in consultation between the cardiologist, surgeon and anaesthetist. The anaesthetist must have sufficient experience of congenital heart diseases to understand their implications for the planned surgery. Patients’ medical history must be checked for episodes of arrhythmia, cardiac decompensation or cyanosis, ischaemic heart disease, renal failure, anaemia and stroke. Preoperatively, some improvements may be achieved through specific cardiological procedures such as percutaneous dilation of the RVOT, radiofrequency ablation of anomalous circuits, embolisation of aortopulmonary collaterals, or assessment of PAH response to NO.
Grown-up congenital heart (GUCH) patients undergo non-cardiac surgical procedures more often than the general population [10]. They present with very special pathologies that call for knowledge that is different from that acquired in the conventional field of cardiology, anaesthesia and cardiac surgery. With the exception of low-risk patients with simple pathologies, it is essential for high-risk patients to be managed at centres of excellence offering cardiology, surgery and intensive care departments dedicated to this field. This applies equally to cardiac and non-cardiac surgery. It is particularly true of cyanotic patients, carriers of complex malformations, patients suffering from PAH, or those experiencing malignant arrhythmias [2,12].
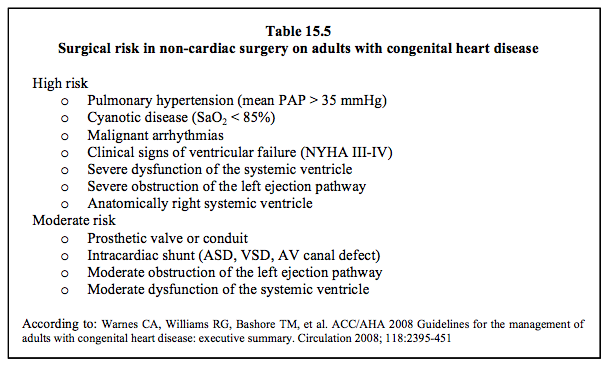
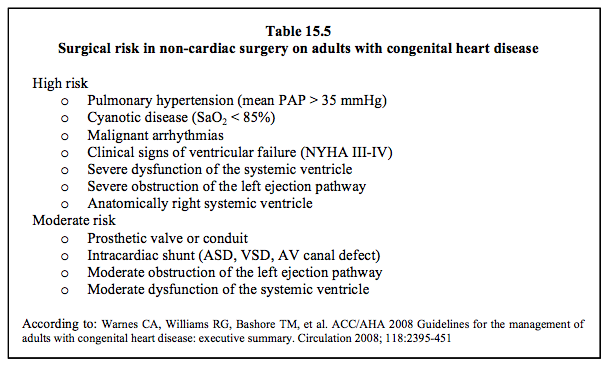
Anaesthetists should ask themselves five key questions before approaching an adult patient with congenital heart disease (Table 15.5):
Grown-up congenital heart (GUCH) patients undergo non-cardiac surgical procedures more often than the general population [10]. They present with very special pathologies that call for knowledge that is different from that acquired in the conventional field of cardiology, anaesthesia and cardiac surgery. With the exception of low-risk patients with simple pathologies, it is essential for high-risk patients to be managed at centres of excellence offering cardiology, surgery and intensive care departments dedicated to this field. This applies equally to cardiac and non-cardiac surgery. It is particularly true of cyanotic patients, carriers of complex malformations, patients suffering from PAH, or those experiencing malignant arrhythmias [2,12].
Anaesthetists should ask themselves five key questions before approaching an adult patient with congenital heart disease (Table 15.5):
- Is there a shunt?
- What is the pulmonary arterial pressure?
- Is the patient cyanotic?
- What is his/her ventricular function?
- What is the risk of arrhythmia?
In a set of 5,265 grown-up congenital heart patients, the most commonly performed operations and reoperations are: surgery on the right ejection pathway and PA (21%), operations for arrhythmias (20%), procedures on the left ejection pathway, aortic valve and aorta (18%), VSD closure (7%), mitral valve surgery (5%), and Fontan surgery (4%) [8].
© BETTEX D, CHASSOT PG, January 2008, last update February 2020
| Anaesthesia for adult congenital heart disease patients |
| Adults with congenital heart disease experience specific problems: - Ventricular dysfunction - High incidence of arrhythmias that respond poorly to medical treatment - Pulmonary circulation anomalies – either excessive (PAH) or insufficient (cyanosis) flow - High thromboembolic risk - Multiple organ failure secondary to cyanosis, hypoxaemia, and haemodynamics - Age-related diseases (diabetes, hypertension, coronary ischaemia, COPD, etc.) Their perioperative mortality is more than double that of the general population. |
© BETTEX D, CHASSOT PG, January 2008, last update February 2020
References
- ANDROPOULOS DB, STAYER SA, SKJONSBY BS, et al. Anesthetic and perioperative outcome of teenagers and adults with congenital heart disease. J Cardiothorac Vasc Anesth 2002; 16:731-6
- BAEHNER T, ELLERKMANN RK. Anesthesia in adults with congenital heart disease. Curr Opin Anaesthesiol 2017; 30:418-25
- CANNESSON M, EARING MG, COLLANGE V, KERSTEN JR. Anesthesia for noncardiac surgery in adults with congenital heart disease. Anesthesiology 2009; 111:432-40
- CHASSOT PG, BETTEX DA. Anesthesia and adult congenital heart disease. J Cardiothorac Vasc Anesth 2006; 20:414-37
- FINDLOW D, DOYLE E. Congenital heart disease in adults. Br J Anaesth 1997; 78:416-30
- HEGGIE J, POIRER N, WILLIAMS WG, KARSKI J. Anesthetic considerations for adult cardiac surgery patients with congenital heart disease. Sem Cardiothorac Vasc Anesth 2003; 7:141-52
- LOVELL AT. Anaesthetic implications of grown-up congenital heart disease. Br J Anaesth 2004; 93:129-39
- MASCIO CE, PASQUALI SK, JACOBS JP, et al. Outcomes in adult congenital heart surgery: analysis of the Society of Thoracic Surgeons database. J Thorac Cardiovasc Surg 2011; 142:1090-7
- REDINGTON A, SHORE D, OLDERSHAW P. Congenital heart disease in adults. A practical guide. London, WB Saunders Co Ltd, 1994, pp 57-66
- ROUINE-RAPP K, RUSSELL IA, FOSTER E. Congenital heart disease in the adult. Int Anesthesiol Clin 2012; 50:16-39
- STOUT KK, DANIELS CJ, VALENTE AM, et al. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease. J Am Coll Cardiol 2019; 73:e81-192
- WARNES CA, WILLIAMS RG, BASHORE TM, et al. ACC/AHA 2008 Guidelines for the management of adults with congenital heart disease: executive summary. Circulation 2008; 118:2395-451
