Whatever the temperature reached during hypothermia period, rewarming should be gradual. The temperature gradient between the water in the heat exchanger circuit and the patient's blood should not exceed 10°C; the difference between oesophageal and rectal temperatures should not exceed 10°C. The maximum blood temperature should not exceed 37°C to avoid cerebral hyperthermia [5,8]. When the temperature is still < 30°C, the temperature gradient between the inlet and outlet of the heat exchanger should not exceed 10°C; as soon as the temperature is > 30°C, this gradient should remain ≤ 4°C. The heating rate should not exceed 0.5°C/min (recommended: 1°C/5 min) [3]. There are four major risks with overheating.
- Temperature inhomogeneity within the tissues; some areas remain cold due to intense arteriolar vasoconstriction.
- Cerebral hyperthermia (38-39°C) leading to worsening neurological disorders.
- Gas embolisms due to the decrease in solubility of gases as the blood heats up.
- Serum protein denaturation.
The warm-up period is a time of major activity for the anaesthetist [1].
- As soon as the warming begins, a deepening of the anaesthesia should be planned. Indeed, conscious cortical activity, absent < 30-32°C, resumes when the brain temperature exceeds this threshold. This temperature evolves more rapidly than the temperature measured in the oesophagus; unconsciousness must therefore be ensured from the start of the warming up procedure. Without a means of measuring brain electrical activity (EEG, BIS™, Entropy™), it is impossible to know whether the patient is adequately asleep, as the usual criteria for anaesthesia are absent in ECC: haemodynamics are machine dependent, sweating is caused by blood warming, and the pupils remain miosis due to high doses of opiates. It is therefore recommended that sleep is provided by midazolam (5-15 mg), propofol (5 mg/kg/hour) or halogen (1-1.5 MAC). The central venodilation caused by propofol usually requires the perfusionist to add 500 mL of crystalloid to the circuit to compensate for the drop in venous return. It is rarely useful to give fentanyl or another opioid at this time unless it is intended to block any sympathetic response that may cause pulmonary hypertension.
- The administration of a curare avoids shivering and decreases muscle O2 consumption, but eliminates the only criterion for awakening, which is spontaneous movement.
- Patients in congestive failure with ventricular dilatation or pulmonary hypertension, in whom inodilation is beneficial, benefit a slow bolus dose of milrinone (Corotrop® ) in the bypass at the time of rewarming [2]; a decrease in systemic pressure is usual during this administration.
- When the aorta is unclamped, coronary perfusion is restored and the heart fibrillates or starts beating spontaneously again, often momentarily anarchically.
- If the heart is in fibrillation, defibrillate one or more times with the internal pads; start with 5-10 J depending on the size of the heart, and increase if necessary. The maximum energy possible with the internal system is 50 J. If success is not immediate, it is usual to add lidocaine (2 mg/kg iv) and magnesium (5-10 mmol). If atrial fibrillation occurs, synchronous cardioversion is performed (5-20 J). If ventricular fibrillation is refractory to any treatment, the heart can be re-cardioplegised and weaning off pump restarted after a recovery period.
- Ventilation is resumed when cardiac activity is restored, if it does not interfere with the operator [7]. This is preceded by vital capacity manoeuvres (30-40 cm H2 O insufflation for 20-30 seconds); the surgical field is carefully monitored during these manoeuvres to avoid interfering with surgical activity or exerting deleterious traction on the mammery graft(s) [4]. When beating, the heart maintains some pulmonary circulation, so it is wise to maintain reduced ventilation by adjusting ventilator parameters to half the beating heart values (FiO25, VC 3-4 mL/kg, rate 5-8 cycles/min) [6,7]. The PetCO2 readout on the ventilator is low, since gas exchange takes place mainly through the oxygenator. Nevertheless, the Fi of the halogen should be identical on both machines to avoid gas entering one and leaving the other.
- In the event of ventricular dysfunction, halogen gas is temporarily discontinued; it will be resumed on the ventilator in the event of coronary revascularisation (preconditioning effect) if ventricular function is adequate.
- Hyperkalaemia (> 5 mmol/L) is common due to the high K+ content of the cardioplegia solutions that are drawn back into the bypass circuit. Ca2+ injection counteracts the effects of potassium. Kaliuria can be forced with mannitol or furosemide. In case of renal failure, cardioplegia is evacuated by "lost" suction or by haemofiltration. Ringer's solution should be replaced by 0.9% NaCl. In the absence of ECG changes, the situation is safe and even beneficial because of the stabilisation of the membranes.
- Inotropic agents should not be given too early before weaning off pump because they increase mVO2 at a time when O2 use by the myocardial cell is still impaired. Ten minutes before weaning off pump is usually enough to achieve an optimal inotropic serum level.
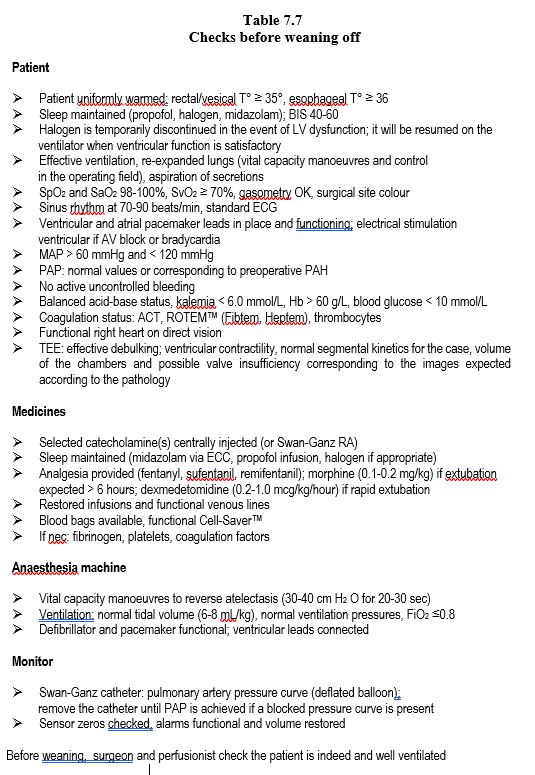
The final preparation for weaning off pump is discussed below in Weaning from ECC and is summarised in Table 7.7.
| Warming up |
| Provide sleep and curarization if necessary
Reventilate as soon as cardiac activity is resumed (if it does not interfere with surgeon activity)
Vital capacity manoeuvre (30-40 cm H2 O for 20-30 seconds)
Slow warming to reach rectal T° ≥ 35°, esophageal T° ≥ 36°.
- Temperature increase 1°C / 5 min
- Blood temperature ≤ 37°C
If VF or VT: defibrillation(s) (internal pads: 5-50 J), xylocaine 2 mg/kg, Mg2+ 2 gm
If AF: cardioversion (internal pads: 5-20 J)
|
© CHASSOT PG, GRONCHI F, April 2008, last update, December 2019
References
- BARRY AE, CHANEY MA, LONDON MJ. Anaesthetic management during cardiopulmonary bypass: a systematic review. Anesth Analg 2015; 120:749-69
- DOOLAN LA, JONES EF, KALMAN J, et al. A placebo-controlled trial verifying the efficacy of milrinone in weaning high-risk patients from cardiopulmonary bypass. J Cardiothor Vasc Anesth 1997; 11:37-41
- ENGELMAN R, BAKER RA, LIKOSKY DS, et al. The Society of Thoracic Surgeons, the Society of Cardiovascilar Anesthesiologists, and the American Society of Extracorporeal Technology: clinical practice guidelines for cardiopulmonary bypass - Temperature management during cardioplmonary bypass. J Cardiothorac Vasc Anesth 2015; 29:1104-13
- GARCIA-DELGADO M, NAVARETTE-SÀNCHEZ I, COLMENERO M. Preventing and managing perioperative pulmonary complications following cardiac surgery. Curr Opin Anesthesiol 2014; 27:146-52
- GRIGORE AM, MURRAY CF, RAMAKRISHNA H, DJAIANI G. A core review of temperature regimens and neuroprotection during cardiopulmonary bypass: does rewarming rate matter? Anesth Analg 2009; 109:1741-51
- MAGNUSSON L, ZEMGULIS V, RENLING A, et al. Use of a vital capacity maneuver to prevent atelectasis after cardiopulmonary bypass. Anesthesiology 1998; 88:134-42
- MURPHY GS, HESSEL EA, GROOM RC. Optimal perfusion during cardiopulmonary bypass: an evidence-based approach. Anesth Analg 2009; 108:1394-417
- SHANN KG, LIKOSKY DS, MURKIN JM, et al. An evidence-based review of the practice of cardiopulmonary bypass in adults: A focus on neurologic injury, glycemic control, hemodilution, and the inflammatory response. J Thorac Cardiovasc Surg 2006; 132:283-90