Ebstein anomaly is characterised by apical displacement of the insertion of the tricuspid valve’s septal and posterior leaflets by over 10 mm (> 0.8 cm/m2) inside the RV (Figure 15.24 and Figure 15.25) (Video).
Video: Dysfunction and dilatation of the partially atrialized right ventricular chamber in a case of Ebstein anomaly; the septal leaflet is inserted too apically on the septum; the very long anterior leaflet is normally inserted, but is incompetent to occlude the tricuspid valve in systole; the posterior leaflet is atretic.
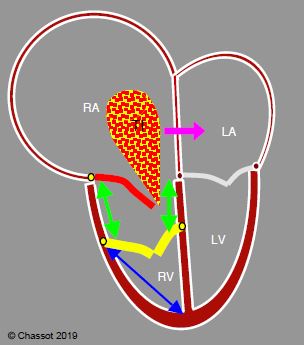
Figure 15.24: Ebstein anomaly. The septal and posterior leaflets of the tricuspid valve (yellow) are inserted low (> 1.5 cm below the insertion of the mitral valve), while the anterior leaflet (red) is in its normal position. The RV inlet is in the RA (green arrows). The RA is highly dilated and the RV is restrictive. Tricuspid insufficiency (TI) is generally severe. If a PFO or ASD is present, the shunt is often R-to-L and cyanotic (pink arrow) because the RA is under high pressure. The ratio of RV atrialisation length (green arrows) to RV functional chamber length (blue arrow) must be < 0.5 in order to perform valve repair. This entails the anterior leaflet either being used as the sole means of closing the valve (single-leaflet valve reconstruction) or in combination with one of the other two leaflets if just one is inserted in a low position (bicuspid reconstruction).
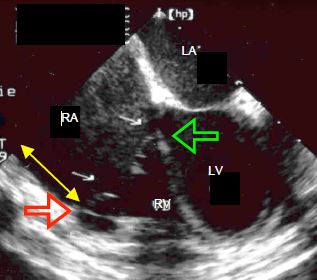
Figure 15.25: Images of an Ebstein anomaly. The arrows show the low insertion position of the posterior (red) and septal (green) leaflets. The yellow double arrow shows the portion of the RV that is atrialised. The RV is small and triangular while the RA is very large.
While both these leaflets exhibit reduced mobility due to shortening and progressive fibrosis of the chordae, the anterior leaflet generally remains flexible, mobile and normally positioned. The right ventricular chamber is small and the RV inlet becomes part of the right atrium. It is consequently described as being “atrialised”. The RA is highly dilated. An ASD is present in > 50% of cases [7]. The RV is highly restrictive despite its rounded appearance. It is dysfunctional (Vidéo Dysf VD Ebstein). The tricuspid valve may be insufficient, stenotic or both. The severity of tricuspid insufficiency can easily be underestimated due to the immensity of the RA and the low velocity of the flow linked to the large size of the regurgitation orifice and/or the right-sided dysfunction, which is itself often underestimated due to ventricular remodelling (Video and Figure 15.26).
Video: Massive tricuspid regurgitation in a case of Ebstein anomaly.
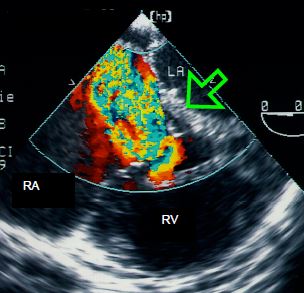
Figure 15.26: Transesophageal echocardiographic view of massive tricuspid insufficiency in a case of Ebstein anomaly. The green arrow shows the low insertion position of the septal leaflet.
Accessory conduction bundles are common, causing Wolff-Parkinson-White arrhythmia. There is little correlation between echocardiographic morphology and the functional impact of the disease [2].
Auscultation reveals a significant split second sound at the lower left border of the sternum and an early tricuspid insufficiency murmur. The disease manifests clinically as a limitation of the right ventricular flow – systemic stasis, hepatomegaly and right-sided congestive failure. Cyanosis occurs in the event of combination with an ASD or PFO (R-to-L shunt). Symptom onset often occurs at the end of adolescence. Without treatment, 80% of patients die before the age of 30 years [1]. In 25-30% of cases, patients exhibit severe arrhythmias in the form of AV blocks and WPW syndrome, which may be the first sign of the disease [5]. Prognosis is linked to functional status, the extent of right-sided failure, the severity of arrhythmias and any cyanosis present.
The size of the trabeculated portion of the RV determines what type of surgical correction is possible. If the RV is satisfactory, the operation involves reduction atrioplasty and tricuspid valve repair transforming the tricuspid into a single-leaflet valve occluded only by the anterior leaflet, or into a bicuspid valve if only one leaflet is inserted in a low position. This is only possible if the anterior leaflet is sufficiently large and mobile and if the functional chamber of the RV is at least a third of its total chamber size. This type of repair gives the valve tissue a conical shape (cone procedure) [4]. Valve replacement cannot always be avoided. If present, the ASD is closed by a patch. If the RV is hypoplastic, dilated or failing, an additional cavopulmonary anastomosis (insertion of the SVC in the right PA, or Glenn shunt) is sometimes necessary to ensure satisfactory pulmonary blood flow, as long as LV end-diastolic pressure is normal [1,6]. In the event of refractory flutters or AFs, this surgery is supplemented by a maze procedure (see Chapter 20, Surgical ablation of AF) [3].
Anaesthesia
Anaesthesia is managed based on two fundamental factors: limitation of RV volume (right-sided restrictive failure) and arrhythmias. RV ejection is facilitated by pulmonary vasodilation (see Table 15.6) and low intrathoracic pressure (low-pressure IPPV). The insertion of a central line may trigger very dangerous arrhythmias, since part of the right atrial wall consists of ventricular wall. Following surgical correction, the tricuspid flow must not be restrictive – the mean gradient through the valve must not exceed 5 mmHg – moderate residual leakage is acceptable. Right-sided dysfunction is common and poorly tolerated. It may require ECMO. Complete AV blocks are not uncommon after tricuspid repair and are managed by a permanent pacemaker [3].
© BETTEX D, CHASSOT PG, January 2008, last update February 2020
References
Video: Dysfunction and dilatation of the partially atrialized right ventricular chamber in a case of Ebstein anomaly; the septal leaflet is inserted too apically on the septum; the very long anterior leaflet is normally inserted, but is incompetent to occlude the tricuspid valve in systole; the posterior leaflet is atretic.
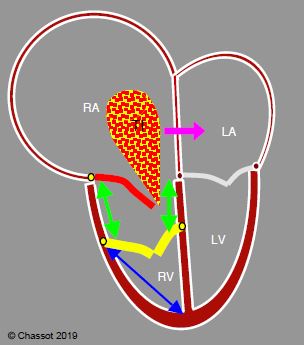
Figure 15.24: Ebstein anomaly. The septal and posterior leaflets of the tricuspid valve (yellow) are inserted low (> 1.5 cm below the insertion of the mitral valve), while the anterior leaflet (red) is in its normal position. The RV inlet is in the RA (green arrows). The RA is highly dilated and the RV is restrictive. Tricuspid insufficiency (TI) is generally severe. If a PFO or ASD is present, the shunt is often R-to-L and cyanotic (pink arrow) because the RA is under high pressure. The ratio of RV atrialisation length (green arrows) to RV functional chamber length (blue arrow) must be < 0.5 in order to perform valve repair. This entails the anterior leaflet either being used as the sole means of closing the valve (single-leaflet valve reconstruction) or in combination with one of the other two leaflets if just one is inserted in a low position (bicuspid reconstruction).
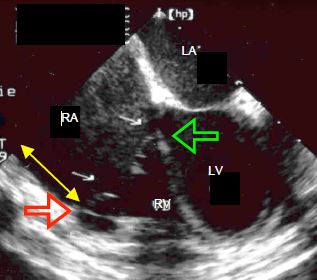
Figure 15.25: Images of an Ebstein anomaly. The arrows show the low insertion position of the posterior (red) and septal (green) leaflets. The yellow double arrow shows the portion of the RV that is atrialised. The RV is small and triangular while the RA is very large.
While both these leaflets exhibit reduced mobility due to shortening and progressive fibrosis of the chordae, the anterior leaflet generally remains flexible, mobile and normally positioned. The right ventricular chamber is small and the RV inlet becomes part of the right atrium. It is consequently described as being “atrialised”. The RA is highly dilated. An ASD is present in > 50% of cases [7]. The RV is highly restrictive despite its rounded appearance. It is dysfunctional (Vidéo Dysf VD Ebstein). The tricuspid valve may be insufficient, stenotic or both. The severity of tricuspid insufficiency can easily be underestimated due to the immensity of the RA and the low velocity of the flow linked to the large size of the regurgitation orifice and/or the right-sided dysfunction, which is itself often underestimated due to ventricular remodelling (Video and Figure 15.26).
Video: Massive tricuspid regurgitation in a case of Ebstein anomaly.
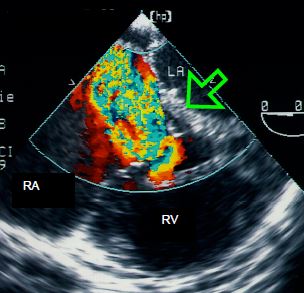
Figure 15.26: Transesophageal echocardiographic view of massive tricuspid insufficiency in a case of Ebstein anomaly. The green arrow shows the low insertion position of the septal leaflet.
Accessory conduction bundles are common, causing Wolff-Parkinson-White arrhythmia. There is little correlation between echocardiographic morphology and the functional impact of the disease [2].
Auscultation reveals a significant split second sound at the lower left border of the sternum and an early tricuspid insufficiency murmur. The disease manifests clinically as a limitation of the right ventricular flow – systemic stasis, hepatomegaly and right-sided congestive failure. Cyanosis occurs in the event of combination with an ASD or PFO (R-to-L shunt). Symptom onset often occurs at the end of adolescence. Without treatment, 80% of patients die before the age of 30 years [1]. In 25-30% of cases, patients exhibit severe arrhythmias in the form of AV blocks and WPW syndrome, which may be the first sign of the disease [5]. Prognosis is linked to functional status, the extent of right-sided failure, the severity of arrhythmias and any cyanosis present.
The size of the trabeculated portion of the RV determines what type of surgical correction is possible. If the RV is satisfactory, the operation involves reduction atrioplasty and tricuspid valve repair transforming the tricuspid into a single-leaflet valve occluded only by the anterior leaflet, or into a bicuspid valve if only one leaflet is inserted in a low position. This is only possible if the anterior leaflet is sufficiently large and mobile and if the functional chamber of the RV is at least a third of its total chamber size. This type of repair gives the valve tissue a conical shape (cone procedure) [4]. Valve replacement cannot always be avoided. If present, the ASD is closed by a patch. If the RV is hypoplastic, dilated or failing, an additional cavopulmonary anastomosis (insertion of the SVC in the right PA, or Glenn shunt) is sometimes necessary to ensure satisfactory pulmonary blood flow, as long as LV end-diastolic pressure is normal [1,6]. In the event of refractory flutters or AFs, this surgery is supplemented by a maze procedure (see Chapter 20, Surgical ablation of AF) [3].
Anaesthesia
Anaesthesia is managed based on two fundamental factors: limitation of RV volume (right-sided restrictive failure) and arrhythmias. RV ejection is facilitated by pulmonary vasodilation (see Table 15.6) and low intrathoracic pressure (low-pressure IPPV). The insertion of a central line may trigger very dangerous arrhythmias, since part of the right atrial wall consists of ventricular wall. Following surgical correction, the tricuspid flow must not be restrictive – the mean gradient through the valve must not exceed 5 mmHg – moderate residual leakage is acceptable. Right-sided dysfunction is common and poorly tolerated. It may require ECMO. Complete AV blocks are not uncommon after tricuspid repair and are managed by a permanent pacemaker [3].
| Ebstein anomaly |
|
Apical insertion of the posterior and septal leaflets of the tricuspid valve with narrowing of the RV chamber, atrialisation of its inlet, dilation of the RA, and tricuspid insufficiency.
Haemodynamics: right ventricular failure (restrictive RV), refractory arrhythmias Anaesthesia: reduce RV afterload (pulmonary vasodilation, low-pressure IPPV), inotropic support of the RV, ECMO if appropriate |
© BETTEX D, CHASSOT PG, January 2008, last update February 2020
References
- BAUMGARTNER H, BONHOEFFER P, DE GROOT NMS, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 2010; 31:2915-57
- BENSON LN, CHILD JS, SCHWAIGER M, et al. Left ventricular geometry and function in adults with Ebstein's anomaly of the tricuspid valve. Circulation 1987; 75:353-9
- BHATT AB, FOSTER E, KUEHL K, et al. Congenital hesart disease in older adult. A Scientific Statement from the American Heart Association. Circulation 2015; 131:1884-931
- DEARANI JA, SAID SM, O'LEARY PW, et al. Anatomic repair of Ebstein's malformation: lessons learned with cone reconstruction. Ann Thorac Surg 2013; 95:220-6
- PERLOFF JK, WARNES CA: Challenges posed by adults with repaired congenital heart disease. Circulation 2001; 103:2637-43
- STOUT KK, DANIELS CJ, VALENTE AM, et al. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease. J Am Coll Cardiol 2019; 73:e81-192
- WARNES CA, WILLIAMS RG, BASHORE TM, et al. ACC/AHA 2008 Guidelines for the management of adults with congenital heart disease: executive summary. Circulation 2008; 118:2395-451
