From fish to birds and mammals, all vertebrates have a complex system of soluble serum proteins that can precipitate and prevent local exsanguination from wounds without causing diffuse coagulation of the circulation. This system is vital because pressurised blood perfusion is the keystone that keeps the body alive.The treatment of many cardiovascular diseases and the introduction of various prostheses in contact with blood have led to a more or less profound slowing down of the natural coagulatory activity, although we are far from fully understanding its subtlety. However effective they may be, our antithrombotic treatments are like an elephant in a shop ! On the other hand, priority of action depends on specialty. For a cardiologist, thrombus is a tragedy ; for a surgeon, it is haemorrhage. It is therefore not surprising that perioperative coagulation management is a subject of intense controversy. Given the multiplicity of possible situations, it is not conceivable to lay down general rules encompassing all of them. Theoretical knowledge and practical experience have certainly made possible general recommendations, but clinical judgement remains essential to find the right balance between thrombotic and haemorrhagic risk in each particular case.
In recent years, a form of practical haematology has become established in the operating theatre, extending the scope of anaesthesia. The ability to perform on-site coagulation (e.g. ROTEM™) and platelet activity testing (e.g. Multiplate™, VerifyNow™, PFA-100™) has paved the way for more rational management of haemostasis and coagulation factors, based on the specific needs of the patient (goal-directed therapy). On the other hand, the arrival on the clinical market of new anticoagulant and antiplatelet agents has changed the perioperative management of patients. Finally, the idea of global management of the patient's blood has gradually integrated the preoperative preparation of the patient, the transfusion of blood and platelets, the administration of plasma derivatives and coagulation factors, and the direct assessment of coagulation performance into a functional whole that requires the anaesthetist to have a good knowledge of haematology. In addition, the anaesthetist involved in cardiac surgery must be able to deal with the anticoagulation problems posed by the use of extracorporeal circulation material.
Future developments in this area will undoubtedly lead to a more coherent management of haemostasis and a more restrictive use of blood products. Thus, algorithms are being developed for the management of patients undergoing surgery with anticoagulants and for the management of different procoagulant products, bearing in mind that the aim is not to normalise the status but to achieve an optimal balance between haemorrhagic and thrombotic risk. This balance point may be at a different point on the spectrum, depending on the risks specific to the patient and the surgical situation.
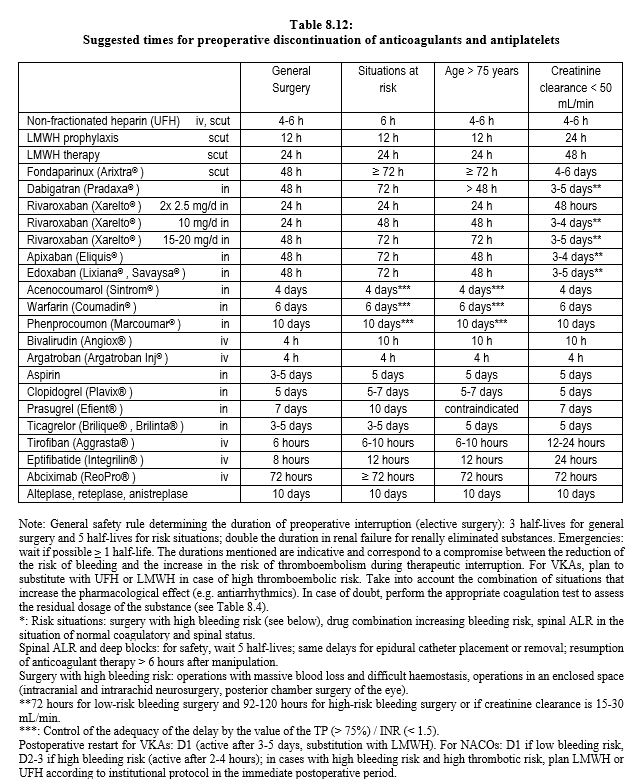
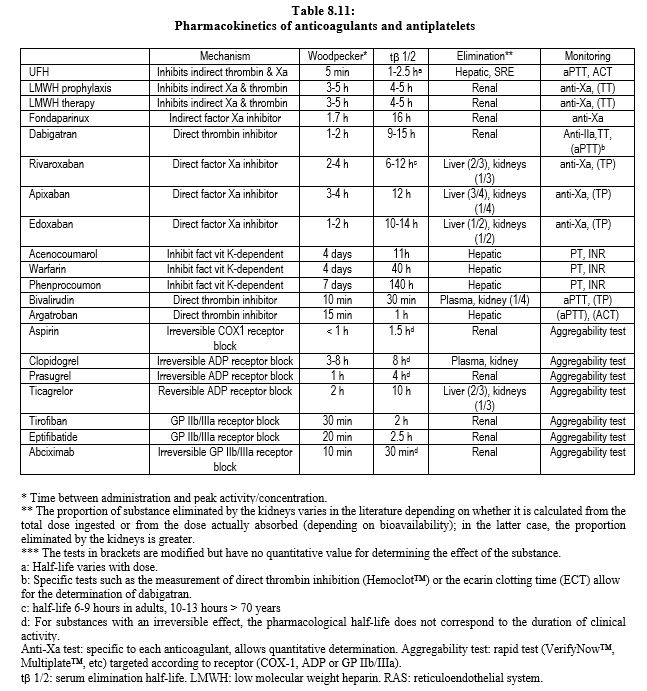
At present, the introduction of new anticoagulants into practice is often confusing for the anaesthetist, who may have some difficulty in navigating the timelines for preoperative discontinuation of treatment, particularly in the case of spinal anesthesia. Tables 8.11 and 8.12 attempt to address this problem by providing a summary of pharmacokinetic data and proposed recommendations for preoperative discontinuation of anticoagulants and antiplatelets agents.
© CHASSOT PG, MARCUCCI Carlo, last update November 2019.