Congenital heart defects appear to be a very esoteric topic. However, these malformations are quite frequent, since they occur in 0.5-1% of births, if we exclude the patent foramen ovale (incidence 20%) and bicuspid aortic valve (incidence 2%). The average prevalence is 0.93% in Asia, 0.82% in Europe, 0.65% in South America and 0.2% in Africa [12]. Complex, rarer malformations appear only in 1‰ of newborns [3].
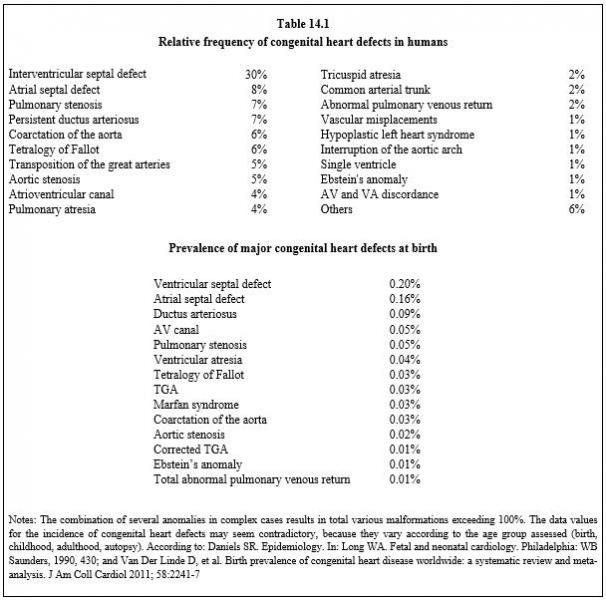
The prevalence in children born to mothers with congenital heart defects themselves is 3% for tetralogy of Fallot, 6-8% for ventricular septal defect and rises to 12% for atrioventricular septal defect [1,10]. Although countless defects may have been described, three-quarters of them involve the following abnormalities: ventricular septal defect (26%), persistent ductus arteriosus (14%), ASD (11%), tetralogy of Fallot (9%), pulmonary stenosis (8%), coarctation of the aorta (6%), transposition of the great arteries (6%) and aortic stenosis (5%) [5.12]. The prevalence of the main malformations is shown in Table 14.1. Congenital heart disease must be considered as a systemic disease, because it is associated in more than a quarter of cases with a host of malformations of the skeleton (dysmorphism and intubation difficulty), of the central nervous system (convulsions), of the respiratory system (restrictive and obstructive lesions), of the liver and kidneys (65% of cyanotic patients suffer from nephropathy) [2].
The prevalence in children born to mothers with congenital heart defects themselves is 3% for tetralogy of Fallot, 6-8% for ventricular septal defect and rises to 12% for atrioventricular septal defect [1,10]. Although countless defects may have been described, three-quarters of them involve the following abnormalities: ventricular septal defect (26%), persistent ductus arteriosus (14%), ASD (11%), tetralogy of Fallot (9%), pulmonary stenosis (8%), coarctation of the aorta (6%), transposition of the great arteries (6%) and aortic stenosis (5%) [5.12]. The prevalence of the main malformations is shown in Table 14.1. Congenital heart disease must be considered as a systemic disease, because it is associated in more than a quarter of cases with a host of malformations of the skeleton (dysmorphism and intubation difficulty), of the central nervous system (convulsions), of the respiratory system (restrictive and obstructive lesions), of the liver and kidneys (65% of cyanotic patients suffer from nephropathy) [2].
Congenital heart defects have numerous several origins and are associated with several phenomena [7,8,11].
- Genetics (detectable in 30% of cases): trisomy 21, 13 and 18, Noonan and Williams syndromes, 22q11 microdeletion, Zic3, FoxH1 or CFC1 mutations, laterality anomalies related to the gene PITX2, transcription errors in differentiation molecules (TGF-β, SMAD), DNA mutations (NKX2.5, MESP1) [7].
- Long list of rare congenital syndromes frequently associated with heart malformations.
- Maternal: rubella, diabetes, lupus or alcoholism in the mother; prescription of thalidomide, of lithium or of various anti-seizure and anti-epilepsy drugs during pregnancy.
- Flow abnormalities: an abnormal intracardiac flow can influence the development of downstream structures.
- Prematurity.
But more often, no direct causal factor directly involved is found, and the process is a matter of a local and random functioning defect in the complex machinery of embryology.
Paediatric heart surgery has made such progress during the last 30 years that operative mortality is now less than 5% globally. The survival rate to adulthood of children operated on for congenital heart defects is on average 80% for complex heart disease and ≥ 98% for simple cases [9,11,12,13]. However, only ductus arteriosus (DA), ostium secundum atrial septal defect (ASD) and an isolated small interventricular septal defect (VSD) allow a total correction without sequelae, provided that they are operated on before the age of 2 years (VSD) to 5 years (ASD) [6]. For the others, the importance of residual lesions depends on the age when the surgical correction took place: The sooner the child is operated on (< 3 years), the less important the sequelae are. For this reason, a total correction rather than a palliative intervention is performed as much as possible in early childhood. Despite the very high surgical risks, this trend provides children with a near-normal quality of life, although 27% of them must undergo a second operation [4.6]. Transposition of the great arteries (TGA) is a good example: the aortopulmonary switch operation carried out during the first three weeks of life allows adequate later development (survival beyond 20 years ≥ 95%), but this is not possible with atrial switch operations (Mustard’s or Senning’s operation) performed 2 or 3 years later (survival after 20 years 56-70%) [6]. The advances in paediatric heart surgery are clearly illustrated by the 16-year survival of children operated on for truncus arteriosus or hypoplasia of the aortic arch: from 20% in the 1970s, it has increased to 95% since the 2000s [6]. Unfortunately, there are also a number of disease which require palliative, often repetitive operations, such as hypoplastic left or right heart syndrome; operations in several stages (Norwood, Fontan) allow life to be prolonged, but do not provide a normal adult life (survival after 20 years: 80%) [6]. Only a heart transplant ensures a complete correction.
Caring for children suffering from a heart defect calls for specialist teams and specific knowledge that is different from that acquired in the conventional field of cardiology, anaesthesia and paediatrics. Nevertheless, even if he/she does not practice in a specialist centre, each anaesthetist may encounter one of these patients during an urgent noncardiac operation such as an appendectomy or a fracture reduction.
This chapter voluntarily emphasises the cardiological and surgical aspects, because only a good understanding of heart disease and its surgical correction allows the anaesthetist to adequately manage caring for the child during the operation. Heart defects are an area where a “one-size-fits-all” attitude is not applicable for anaesthesia. As chapters 14 and 15 deal with the same diseases but at different ages, it is inevitable that they overlap extensively and that they contain repetitions of each other.
Paediatric heart surgery has made such progress during the last 30 years that operative mortality is now less than 5% globally. The survival rate to adulthood of children operated on for congenital heart defects is on average 80% for complex heart disease and ≥ 98% for simple cases [9,11,12,13]. However, only ductus arteriosus (DA), ostium secundum atrial septal defect (ASD) and an isolated small interventricular septal defect (VSD) allow a total correction without sequelae, provided that they are operated on before the age of 2 years (VSD) to 5 years (ASD) [6]. For the others, the importance of residual lesions depends on the age when the surgical correction took place: The sooner the child is operated on (< 3 years), the less important the sequelae are. For this reason, a total correction rather than a palliative intervention is performed as much as possible in early childhood. Despite the very high surgical risks, this trend provides children with a near-normal quality of life, although 27% of them must undergo a second operation [4.6]. Transposition of the great arteries (TGA) is a good example: the aortopulmonary switch operation carried out during the first three weeks of life allows adequate later development (survival beyond 20 years ≥ 95%), but this is not possible with atrial switch operations (Mustard’s or Senning’s operation) performed 2 or 3 years later (survival after 20 years 56-70%) [6]. The advances in paediatric heart surgery are clearly illustrated by the 16-year survival of children operated on for truncus arteriosus or hypoplasia of the aortic arch: from 20% in the 1970s, it has increased to 95% since the 2000s [6]. Unfortunately, there are also a number of disease which require palliative, often repetitive operations, such as hypoplastic left or right heart syndrome; operations in several stages (Norwood, Fontan) allow life to be prolonged, but do not provide a normal adult life (survival after 20 years: 80%) [6]. Only a heart transplant ensures a complete correction.
Caring for children suffering from a heart defect calls for specialist teams and specific knowledge that is different from that acquired in the conventional field of cardiology, anaesthesia and paediatrics. Nevertheless, even if he/she does not practice in a specialist centre, each anaesthetist may encounter one of these patients during an urgent noncardiac operation such as an appendectomy or a fracture reduction.
This chapter voluntarily emphasises the cardiological and surgical aspects, because only a good understanding of heart disease and its surgical correction allows the anaesthetist to adequately manage caring for the child during the operation. Heart defects are an area where a “one-size-fits-all” attitude is not applicable for anaesthesia. As chapters 14 and 15 deal with the same diseases but at different ages, it is inevitable that they overlap extensively and that they contain repetitions of each other.
| Congenital heart defects in children |
| The prevalence of congenital heart defects is 0.8% of births (1‰ for complexcases). Currently, surgery offers a survival rate to adulthood of 90% for complex heart disease and ≥ 98% for simple cases. A heart disease operated on is acorrected heart disease, but not a healed heart disease. Only simple ductus arteriosus, ASD and VSD operated on before the age of 3 allow a future without sequelae. |
© BETTEX D, BOEGLI Y, CHASSOT PG, June 2008, last updated February 2020
References
- BAUMGARTNER H, BONHOEFFER P, DE GROOT NMS, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 2010; 31:2915-57
- BHATT AB, FOSTER E, KUEHL K, et al. Congenital hesart disease in older adult. A Scientific Statement from the American Heart Association. Circulation 2015; 131:1884-931
- BRICKNER EM, HILLIS LD, LANGE RA. Congenital heart disease in adults. First of two parts. N Engl J Med 2000; 342:1-12
- CASTANEDA AR, JONAS RA, MAYER JE, HANLEY FL. Cardiac Surgery of the Neonate and Infant. Philadelphia:WB Saunders, 1994, 23
- DANIELS SR. Epidemiology. In: LONG WA. Fetal and neonatal cardiology. Philadelphia: WB Saunders, 1990, 430
- ERIKSSEN G, LIESTOL K, SEEM E, et al. Achievements in congenital heart defect surgery: a prospective, 40-year study of 7'038 patients. Circulation 2015; 131:337-46
- KLOESEL B, DINARDO JA, BODY SC. Cardiac embryology and molecular mechanisms of congenital heart disease – A primer for anesthesiologists. Anesth Analg 2016; 123:551-69
- KUSSMAN BD, HOLZMAN RS. Cardiac embryology : Understanding congenital heart disease for the noncardiac anesthesiologist. Sem Cardiothorac Vasc Anesth 2001 ; 5 : 2-20
- MARELLI AJ, MACKIE AS, IONESCU-ITTU R, et al . Congenital heart disease in the general population: changing prevalence and age distribution. Circulation 2007; 115:163-72
- SILVERSIDES CK, DORE A, POIRIER N, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: Shunt lesions. Can J Cardiol 2010; 26:e70-e79
- TRIEDMAN JK, NEWBURGER JW. Trends in congenital heart disease. The next decade. Circulation 2016; 133:2716-33
- VAN DER LINDE D, KONINGS EE, WITZENBURG M, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 2011; 58:2241-7
- WARNES CA, LIBERTHSON R, DANIELSON GK, et al: Task Force 1: The changing profile of congenital heart disease in adult life. J Am Coll Cardiol 2001; 37:1170-5
