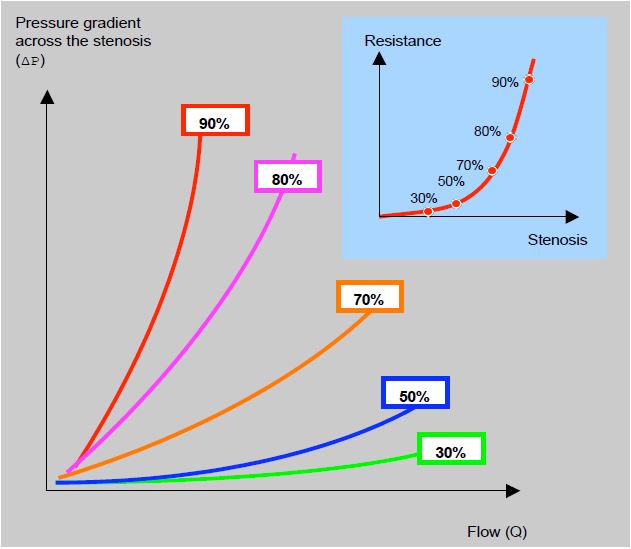
Figure 5.139: Relationship between flow and pressure gradient across a stenosis. The curves illustrate the relationship for different degrees of stenosis in a 3 mm diameter vessel. On the cartouche the curve shows the variation in resistance created by the stenosis as a function of the degree of stenosis. The curves are exponential. This is because the resistance of a fluid in a tube is a function of the fourth power of its radius (Poiseuille's law): Klocke FJ. Measurement of coronary blood flow and degree of stenosis: Current clinical implications and remaining uncertainties. News Council Clin Cardiol AHA 1982].
The pressure gradient across a stenosis increases with the square of the velocity (Bernoulli's law), so resistance increases exponentially as blood flow increases. Therefore, a stress test that accelerates flow can objectively demonstrate the onset of symptoms in a patient who claims to have none. In general, symptoms of valvular stenosis occur before ventricular decompensation, whereas heart failure is characterised by functional deterioration of the LV that precedes the onset of clinical symptoms.
Improvements in surgical outcomes over the last twenty years and the ability to perform a valvuloplasty rather than a valve replacement have led to intervention earlier in the course of the disease, when patients are paucisymptomatic and ventricular function is little altered. Under these conditions, a stress test often reveals myocardial damage that is silent at rest. In the case of aortic stenosis, for example, ergometry or dobutamine stress echo can be used to determine the indication for surgery in three different circumstances [6,8].
- Ischaemic myocardial hibernation;
- Paucisymptomatic valve disease;
- Tight stenosis but low pressure gradient (≤ 30 mmHg).
In the first case, the hypokinesia or akinesia is reversible and will benefit from coronary revascularisation. In the second case, the occurrence of dyspnoea, angina or hypotension during exercise indicates the need for valve replacement. In fact, an abnormal test (symptoms, ST changes, gradient increase > 18 mmHg or blood pressure increase < 20 mmHg) is an independent factor for morbidity and mortality at 2 years [3]. In the third case, the problem is to determine which of the two possibilities is present:
- Tight organic aortic stenosis associated with left ventricular failure secondary to or exacerbated by excessive afterload;
- Functional aortic stenosis due to the inability of the failing LV to properly open a valve that is simply sclerosed.
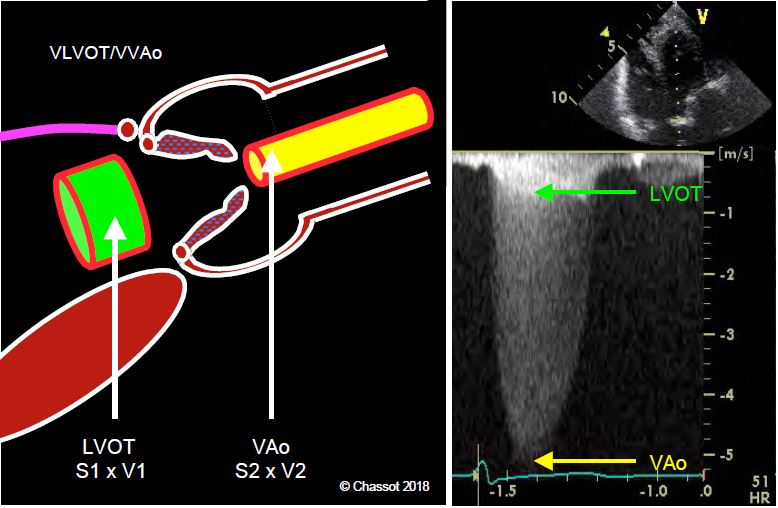
An examination at rest, whether by echocardiography, CT or MRI, cannot distinguish between the two situations, which have very different therapeutic sanctions. In fact, aortic valve replacement (AVR) is beneficial in the first case (5-year survival 65%, compared with 11% for medical treatment), but not in the second, where treatment is for ventricular failure [10]. The situation is clarified by examining the relationship between the velocity in the LV outflow tract (VLVOT ) and that across the aortic valve (VVAo ) during a dobutamine stress echo (infusion 5-10 mcg/kg/min) (Figure 11.30) [1,2,5,7].
- If the stenosis is organic and fixed, the orifice remains unchanged, but Vmax and gradient across the valve increase under the influence of dobutamine (≥ 4 m/s and > 30-40 mmHg, respectively). Under stress, the VLVOT / VVAo ratio continues to widen in a tight stenosis because VTIVAo increases more than VTILVOT; it becomes < 0.2.
- If the stenosis is functional, the valve orifice becomes larger but the transvalvular gradient does not change. The increase in LV contractility leads to an increase in Vmax in the LVOT (from 0.6 to 1.0 m/s), but not in the aortic valve (3 m/s), because the latter opens wider under the effect of the greater stroke volume without increasing its gradient; the VLVOT / VVAo therefore increases (> 0.3).
- The test, which can be performed in the operating theatre, also allows the contractile reserve of the LV to be assessed; the prognosis is improved if the stroke volume increases by > 20%.
- Exertional dyspnoea that is disproportionate to the size of the resting MI;
- Episodes of APO with no apparent cause;
- Moderate MI prior to surgical revascularisation.
| Stress test |
| In the context of valvulopathy, dobutamine stress echo is very useful in determining the indication for surgery in 3 circumstances:
- Paucisymptomatic patients
- Narrow stenosis but low transvalvular gradient
- Myocardial hibernation
The indication for surgery is confirmed when the stress test shows that
- Systolic PAP increases to > 60 mmHg in mitral stenosis or regurgitation; the gradient increases to gradient increases to > 15 mmHg in mitral stenosis
- The gradient increases across the aortic valve; if the stenosis is functional, the ventricle opens further under dobutamine.Left valve opens further under dobutamine and gradient remains unchanged
- Hypokinesia/akinesia is reversible with dobutamine
|
References
- BAUMGARTNER H, FALK V, BAX JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 2017; 38:2739-86
- GRAYBURN PA. Assessment of low-gradient aortic stenosis with dobutamine. Circulation 2006; 113:604-6
- LANCELLOTTI P, LEBOIS F, SIMON M, et al. Prognostic significance of quantitative exercise Doppler echocardiography in asymptomatic aortic valve stenosis. Circulation 2005; 112 Suppl I:I1377-82
- LANCELLOTTI P, TROISFONTAINES P, TOUSSAINT AC, et al. Prognostic significance of exercise-induced changes in mitral regurgitation in patients with chronic ischaemic left ventricular dysfunction. Circulation 2003; 108:1713-7
- LASKEY WK, KUSSMAUL WG, NOORDEGRAAF A. Systemic arterial response to exercise in patients with aortic valve stenosis. Circulation 2009, 119:996-1004
- LIN SS, ROGER VL, PASCOE R, et al. Dobutamine stress Doppler haemodynamics in patients with aortic stenosis: feasibility, safety, and surgical implications. Am Heart J 1998; 136:1010-6
- NISHIMURA RA, OTTO CM, BONOW RO, et al. 2014 AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease. Circulation 2014; 129:e521-e643
- PICANO E, PIBAROT P, LANCELLOTTI P, et al. The emerging role of exercise testing and stress echocardiography in valvular heart disease. J Am Coll Cardiol 2009; 54:2251-60
- PIERARD LA, LANCELLOTTI P. Stress testing in valvular heart disease. Heart 2007; 93:766-72
- TRIBOUILLOY C, LEVY F, RUSINARU D, et al. Outcome after aortic valve replacement for low-flow/low-gradient aortic stenosis without contractile reserve on dobutamine stress echocardiography. J Am Coll Cardiol 2009; 53:1865-73
- VAHANIAN A, ALFIERI O, ANDREOTTI F, et al. Guidelines for the management of valvular heart disease (2012 version). Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2012; 33:2451-96