Principles of anaesthesia:
- High preload;
- Normal rate;
- Contractility: support necessary, but risk of angina if mVO2 is too high;
- Systemic resistance: low if insufficiency predominates (rare), maintained or high if stenosis predominates (usual);
- Pulmonary resistance: normal;
- Tolerance to IPPV: test with Valsalva manoeuvre before induction.
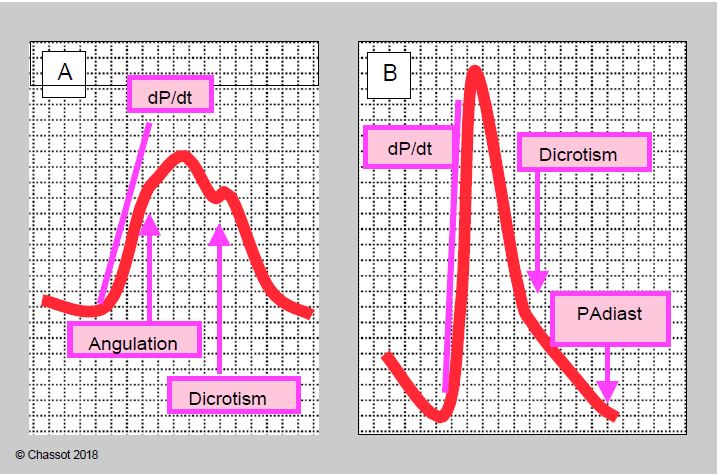
During induction of a patient with aortic disease, the most delicate problem for the anaesthetist is how to manage hypotension. An alpha vasoconstrictor is required if stenosis is predominant, but may decompensate for insufficiency; filling and beta effect are recommended for insufficiency, whereas rhythmic acceleration is detrimental for stenosis. In the setting of aortic replacement surgery, failure to respond to neosynephrine (2-3 consecutive boluses of 100 mcg) should immediately raise the suspicion of a significant component of failure. As it is not always possible to determine the dominant condition from the tests in the patient's record, analysis of the blood pressure curve is a good guide (Figure 11.147):
- In the case of stenosis, dP/dt is reduced, may be angulated as it rises due to the limited opening of the valve, the peak is more rounded and the pulse amplitude is low (pulsus parvus et tardus);
- In failure, the dP/dt is steeper, the curve is sharp, diastolic dicrotism is absent and diastolic pressure is very low (< 50 mmHg); the pulse amplitude is very large (pulsus altus et celer).
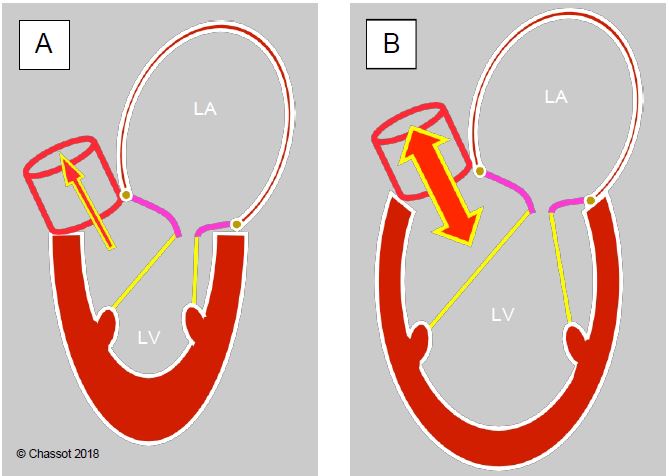
Echocardiography will obviously provide the most relevant answer by visualising the valve, the flows and the remodelling of the left ventricle: small hypertrophied ventricle in stenosis, large dilated ventricle in insufficiency. In the examinations the patient has already undergone, the size of the left ventricle is the most important element in determining the main obstruction (Figure 11.148).
Video: 130° long-axis view of aortic disease with tight stenosis and minor insufficiency.
Video: Transgastric 120° long-axis view of aortic disease (tight stenosis and minor insufficiency).
Figure 11.147: Changes in the silhouette of the arterial curve in predominant aortic stenosis or insufficiency. A: Predominant stenosis; the dP/dt is decreased, angulated, the peak is rounded, the amplitude is small. B: dominant insufficiency; dP/dt is rectified, peak is sharp, diastolic dicrotism is absent, diastolic pressure is low; pulse amplitude is very large.
Figure 11.148: Changes of the cardiac silhouette on echocardiography in aortic disease with predominant stenosis (A) or insufficiency (B). A: Concentric LVH, small ventricular cavity, dilated LV (diastolic dysfunction). B: Dilatative LVH, large ventricular cavity, moderately enlarged LA.
| Hemodynamics sought in aortic disease |
|
High preload |
© CHASSOT PG, BETTEX D, August 2011, last update November 2019
References
- NISHIMURA RA, OTTO CM, BONOW RO, et al. 2014 AHA/ACC Guideline for the management of patients with valvular heart disease. Circulation 2014; 129:e521-e643
- UNGER P, CLAVEL MA, LINDMAN BR, et al. Pathophysiology and management of multivalvular disease. Nat Rev Cardiol 2016; 13:429-40