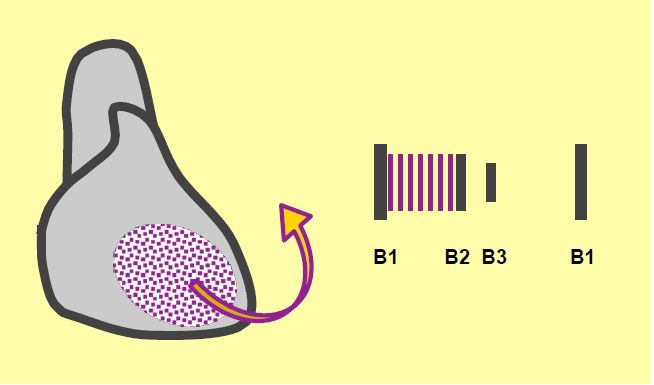
As patients gradually reduce their activity, they do not always complain of fatigue. The best criterion is to ask about the most vigorous activity they can do. Auscultation will reveal a constant high-pitched apical pansystolic murmur radiating in the direction of the MI jet, generally towards the left axillary region (Figure 11.72). In prolapse and rupture, the radiation may be different depending on the orientation of the MI. There is little correlation between the intensity of the murmur and the severity of the insufficiency [2]. As the regurgitant volume returns to the ventricle in diastole, the anterograde mitral flow is increased and accelerated, often resulting in a high-flow diastolic murmur. The pulse is rapid and hyperdynamic. The ECG shows evidence of left ventricular hypertrophy and wide P waves in DII, bifid in V1. A stress test such as the 6-minute walk or dobutamine stress echo often leads to reclassification of asymptomatic patients from stage C (asymptomatic, with or without ventricular dysfunction) to stage D (symptomatic). A reduction in LV size on dobutamine indicates some functional reserve and a good prognosis, in contrast to worsening symptoms and MI, which indicate a decompensated state [9].
Medical therapy is limited in organic MI; vasodilators are only beneficial in functional or ischaemic MI. Atrial fibrillation requires systemic anticoagulation (dicoumarin for INR 2-3) and ventricular failure requires treatment of heart failure [8]. The presence of a secondary MI is a poor prognostic factor, and worsening prognosis is directly proportional to the size of the mitral leak.
The prognosis of mitral insufficiency is determined by a number of factors [9].
- Factors associated with regurgitation
- Severity of the MI;
- Chords rupture, deformation of structures;
- Multiple leaflet damage;
- Secondary MI.
- Clinical factors:
- Age;
- Functional class, severity of symptoms;
- Coronary artery disease;
- Ventricular failure;
- Delay in intervention relative to onset of decompensation.
- LV and LA related factors:
- EF < 60%;
- LV dilatation (telesystolic diameter > 4.0 cm);
- LA dilatation (volume > 60 mL/m2).
- Haemodynamic factors:
- Atrial fibrillation;
- Pulmonary hypertension.
Clinically, mitral insufficiency is divided into 4 progressive stages, analogous to those of ventricular insufficiency [8,9].
- Stage A: Presence of risk factors for the development of MI (e.g. Barlow's disease);
- Stage B: Presence of moderate MI with progressive factors;
- Stage C: severe asymptomatic MI;
- C1: preserved ventricular function
- C2: ventricular decompensation and/or remodelling;
- Stage D: severe symptomatic MI.
Functional examination
Contractility deteriorates progressively under very favourable loading conditions: ejection fraction (EF), which is particularly dependent on afterload, is an ineffective predictor of postoperative function [7]. An EF of 0.6 is no guarantee of preserved function, and a value of 0.5 already indicates significant impairment of systolic performance [4,10]. An EF of 0.4 indicates severe dysfunction that is unlikely to be significantly improved by surgical correction [3,7].
LV telesystolic dimensions correlate best with function and postoperative survival [5]. A normal telesystolic volume (LV diameter < 2.5 cm/m2 or < 4 cm) corresponds to good contractility and a good postoperative prognosis (mortality ≤ 1%), whereas a diameter > 3.0 cm/m2 indicates significant ventricular dysfunction and no longer ensures functional recovery after surgical correction (operative mortality 5-6%) [5,6,7]. For example, after mitral valve surgery, the incidence of left ventricular dysfunction is 9% when the LV telesystolic diameter is < 3.7 cm and 33% when it is > 3.7 cm [11].
In summary, the clinical features of mitral insufficiency are as follows
| Characteristics of mitral insufficiency |
| High preload (LV volume overload) Low afterload (MI leaks when PLV > P LA) LV dilatation (telediastolic diameter > 7 cm or > 4 cm/m2) Impaired systolic function despite preserved EF Criterion for LV dysfunction: telesystolic diameter > 4 cm (> 2.5 cm/m2) MI increases when : RAS ↑ , Vtd ↑ , contractility ↓ Systemic CO dependent on low SAR Intolerance to hypovolemia |
References
- BONOW RO, BRAUNWALD E. Valvular heart disease. In: ZIPES DP, et al, eds. Braunwald's heart disease. A textbook of cardiovascular medicine. 7th edition. Philadelphia: Elsevier Saunders, 2005, 1553-632
- BRAUNWALD E. Valvular heart disease. In: BRAUNWALD E. ed. Heart disease. Philadelphia, WB Saunders Co, 1997, 1007-76
- DI SALVO TG, ACKER MA, DEC GW, BYRNE JG. Mitral valve surgery in advanced heart failure. J Am Coll Cardiol 2010; 55: 271-82
- ENRIQUEZ-SARANO M, TAJIK AK, SCHAFF HV, et al. Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation. Circulation 1994; 90:830-6
- FLEMMING MA, ORAL H, ROTHMAN ED, et al. Echocardiographic markers for mitral valve surgery to preserve left ventricular performance in mitral regurgitation. Am Heart J 2000; 140:476-82.
- FOSTER E. Mitral regurugitation due to degenerative mitral-valve disease. N Engl J Med 2010; 363:156-65
- MATSUMURA T, OHTAKI E, TANAKA K, et al. Echocardiographic prediction of left ventricular dysfunction after mitral valve repair for mitral regurgitation as an indicator to decide the optimal timing of repair. J Am Coll Cardiol 2003; 42:458-66
- NISHIMURA RA, OTTO CM, BONOW RO, et al. 2014 AHA/ACC Guideline for the management of patients with valvular heart disease. Circulation 2014; 129:e521-e643
- O'GARA PT, GRAYBURN PA, BADHWAR V, et al. 2017 ACC Expert consensus decision pathway on the management of mitral regurgitation. J Am Coll Cardiol 2017; 70:2421-49
- TIMMIS SB, KIRSH MM, MONTGOMERY DG, STARLING MR. Evaluation of left ventricular ejection fraction as a measure of pump performance in patients with chronic mitral regurgitation. Cathet Cardiovasc Intervent 2000; 49:290-7
- TRIBOUILLOY C, RUSINARU D, SZYMANSKI C, et al. Predicting left ventricular dysfunction after valve repair for mitral regurgitation due to leaflet prolapse: additive value of left ventricular end-systolic dimension to ejection fraction. Eur J Echocardiogr 2011 ; 12 :702-10
