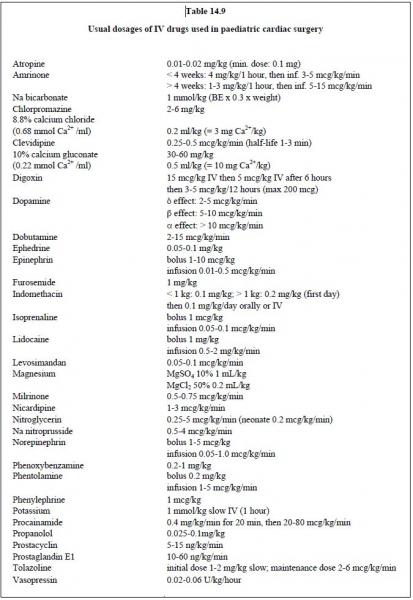
There are three objectives for drug therapy provided to patients with congenital heart diseases (Table 14.9) [3]:
- 1) Optimise cardiac output;
- 2) Maintain organ perfusion pressure;
- 3) Maintain an optimal balance between pulmonary and systemic blood flow. (Qp/Qs = 1).
See Chapter 4 - Cardiovascular medications for further details of haemodynamic pharmacology.
Inotropic agents
Epinephrin is an α1, β1 and β2 stimulant. At low doses, it has a positive inotropic effect (β1). At medium doses, this is combined with an arteriolar vasodilator effect (β2). At high doses, the vasoconstrictor effect (α1) is dominant. Intense vasoconstriction threatens renal and splanchnic perfusion. The β2 effect causes metabolic acidosis and hyperglycaemia. The recommended doses are:
- Bolus: 1-10 mcg/kg every 3-5 minutes with increasing doses (0.1-0.2 mg/kg);
- Infusion 0.01 - 0.5 mcg/kg/min.
At low doses (< 3 mcg/kg/min), dopamine stimulates the dopamine receptors (δ). At moderate doses (5 mcg/kg/min), the β1 effect is predominant. However, above 10 mcg/kg/min, vasoconstriction α is the main component. It is usually recommended to not exceed a dose of 5 mcg/kg/min. If the effect is insufficient, another substance combination should preferably be chosen (dobutamine + norepinephrin, epinephrin + milrinone).
Dobutamine (Dobutrex®) has a preferential activity toward the ß1 receptors (dosage: 2-15 mcg/kg/min). If the β1 receptors are down-regulated (chronic ventricular failure, dobutamine treatment > 72 hours), the efficacy of the substance diminishes. It induces significant tachycardia in young children.
Isoprenaline (Isuprel®) is a β1 and β2 stimulant. It has positive inotropic and chronotropic effects and prompts arteriolar vasodilation. It is mainly used for treating bradycardia and conduction block. Dosage:
Dobutamine (Dobutrex®) has a preferential activity toward the ß1 receptors (dosage: 2-15 mcg/kg/min). If the β1 receptors are down-regulated (chronic ventricular failure, dobutamine treatment > 72 hours), the efficacy of the substance diminishes. It induces significant tachycardia in young children.
Isoprenaline (Isuprel®) is a β1 and β2 stimulant. It has positive inotropic and chronotropic effects and prompts arteriolar vasodilation. It is mainly used for treating bradycardia and conduction block. Dosage:
- Bolus: 1 mcg/kg;
- Infusion: 0.01 - 0.2 mcg/kg/min.
Milrinone (Corotrop®) is a phosphodiesterase-3 inhibitor. It is an inodilator that maintains its inotropic action even if the β1 receptors are depleted. It increases cardiac output by 30%, but reduces PVR and SVR by 25-30% [2]. Its effect is linked with arterial hypotension. It is indicated for patients who benefit from reduced afterload (valvular insufficiency, ventricular dilation) and reduced PVR (R-to-L shunt). It is particularly effective when combined with epinephrin since their cellular points of impact are complementary. Dosage:
- Bolus: 50 mcg/kg (during CPB);
- Infusion: 0.25-0.75 mcg/kg/min;
- Neonates: 0.2 mcg/kg/min (reduced clearance).
Levosimendan (Sindax®) sensitises troponin C to calcium. It has positive inotropic, positive lusitropic, and arterial vasodilator effects. It does not trigger tachycardia, arrhythmia or increased mVO2. Perioperatively, it plays a preconditioning role as it has an anti-ischaemic effect and protects against stunning [5,6,10]. Despite its considerable cost, it is increasingly used in paediatrics as it has virtually no adverse effects [11]. However, it is not officially recommended for prescription to young children [4]. Dosage: 0.05-0.1 mcg/kg/min.
Calcium is useful in cases of hypocalcaemia or at the end of CPB for counteracting hyperkalaemia. Given neonates’ immature Ca2+ release/uptake systems, IV calcium (5-10 mg/kg/h) may have some degree of inotropic effect in very young children.
Digoxin is the most frequently used chronic agent for treating cardiac failure in children. It increases intramyocardial levels of Ca2+ and stimulates the parasympathetic system (bradycardia, conduction block). Dosage:
Calcium is useful in cases of hypocalcaemia or at the end of CPB for counteracting hyperkalaemia. Given neonates’ immature Ca2+ release/uptake systems, IV calcium (5-10 mg/kg/h) may have some degree of inotropic effect in very young children.
Digoxin is the most frequently used chronic agent for treating cardiac failure in children. It increases intramyocardial levels of Ca2+ and stimulates the parasympathetic system (bradycardia, conduction block). Dosage:
- Initial dose: 15 mcg/kg IV then 5 mcg/kg IV after 6 hours;
- Maintenance: 3-5 mcg/kg/12 hours.
Vasoconstrictors
Norepinephrin has a significant α1 stimulating effect and a slight β1 and β2 stimulating effect. Since there are few α receptors in the pulmonary system, norepinephrin increases SVR but has little impact on PVR. It is often required for maintaining coronary perfusion pressure in cases of RV dysfunction with pulmonary hypertension. Dosage:
- Bolus: 1-5 mcg/kg;
- Infusion: 0.05-1.0 mcg/kg/min
Vasopressin is a powerful vasoconstrictor whose effect is not dependent on the α receptors. It is rarely used in paediatrics. The dosage is 0.02-0.06 U/kg/hour [8].
Phenylephrine is a pure α peripheral vasoconstrictor with no combined β effect. Consequently, it increases LV afterload without any concomitant inotropic support. It is useful for increasing SVR in case of hypoxic crises in R-to-L shunts. It is administered as a repeated bolus at a dose of 2-10 mcg/kg.
Systemic vasodilators
Vasodilators are useful for adjusting SVR to achieve Qp:Qs balance, counteracting increases in SVR after hypothermic CPB, and reducing ventricular afterload. Phentolamine (Regitine®) blocks the α1 and α2 receptors and quickly lowers SVR, although it triggers tachycardia. Dosages: bolus 0.2 mg/kg, infusion 1-5 mcg/kg/min. Chlorpromazine is an α blocker with a significant sedative effect (2-6 mg/kg). However, it is outdated. Phenoxybenzamine is an α1 vasodilator that has been used regularly in paediatric cardiac surgery at some centres [12]. It is long-acting as it blocks the systemic receptors irreversibly and significantly lowers SVR. Initial dose: 0.25-1.0 mg/kg. Only vasopressin is capable of inhibiting its hypotensive effect [4].
Two calcium channel blockers are effective arterial vasodilators. However, they exhibit some degree of negative inotropic effect and must be used cautiously in neonates. Nicardipine has a half-life of 40-60 minutes – initial dose 5 mcg/kg/min, followed by a maintenance dose of 1-3 mcg/kg/min. Clevidipine is faster (1-3 minute half-life) and is administered at a rate of 0.25-0.5 mcg/kg/min (max 5 mcg/kg/min) [4].
Nitroglycerin and sodium nitroprusside (Nipruss®) provide NO•. Nitogylcerin preferentially vasodilates the great central veins (capacitance vessels) while sodium nitroprusside's action is chiefly focused on the resistance vessels. Only nitroglycerin is used as a pulmonary vasodilator, since sodium nitroprusside leads to excessive systemic hypotension. Dosage: 0.5-5.0 mcg/kg/min.
Pulmonary vasodilatators
Pulmonary vasodilators include inhaled agents (NO, prostaglandins, milrinone), intravenous substances (prostaglandins, milrinone, sildenafil) and oral medications used in chronic treatment (see Table 14.7 and Paediatric Pulmonary Hypertension) [1].
NO is indicated for persistent pulmonary hypertension in neonates and also for numerous paediatric congenital heart diseases, extending into the postoperative phase following cardiac surgery (RV failure, heart transplant, Fontan physiology, etc.). Dosage: 10-20 ppm in the inspiratory circuit. Side effects: methaemoglobinaemia, NO2 formation, platelet aggregation inhibition, rebound effect on treatment discontinuation.
Sildenafil is a phosphodiesterase-5 inhibitor, which is available in intravenous form. Although the IV form has not been officially approved, it is increasingly used in three scenarios: preventing postoperative PAH crises, treating right-side failure, and discontinuing NO [1]. Dosage: 0.35 mg/kg over 20 minutes, repeated 3 times per day.
Prostaglandins act by stimulating adenylyl cyclase, increase cAMP levels, and prompt quite selective vasodilation of the pulmonary system. They are inhaled or administered intravenously as a chronic or acute treatment and exhibit an additive effect with NO• in reducing PVR in cases of PAH and lowering RV afterload [7,9].
Phenylephrine is a pure α peripheral vasoconstrictor with no combined β effect. Consequently, it increases LV afterload without any concomitant inotropic support. It is useful for increasing SVR in case of hypoxic crises in R-to-L shunts. It is administered as a repeated bolus at a dose of 2-10 mcg/kg.
Systemic vasodilators
Vasodilators are useful for adjusting SVR to achieve Qp:Qs balance, counteracting increases in SVR after hypothermic CPB, and reducing ventricular afterload. Phentolamine (Regitine®) blocks the α1 and α2 receptors and quickly lowers SVR, although it triggers tachycardia. Dosages: bolus 0.2 mg/kg, infusion 1-5 mcg/kg/min. Chlorpromazine is an α blocker with a significant sedative effect (2-6 mg/kg). However, it is outdated. Phenoxybenzamine is an α1 vasodilator that has been used regularly in paediatric cardiac surgery at some centres [12]. It is long-acting as it blocks the systemic receptors irreversibly and significantly lowers SVR. Initial dose: 0.25-1.0 mg/kg. Only vasopressin is capable of inhibiting its hypotensive effect [4].
Two calcium channel blockers are effective arterial vasodilators. However, they exhibit some degree of negative inotropic effect and must be used cautiously in neonates. Nicardipine has a half-life of 40-60 minutes – initial dose 5 mcg/kg/min, followed by a maintenance dose of 1-3 mcg/kg/min. Clevidipine is faster (1-3 minute half-life) and is administered at a rate of 0.25-0.5 mcg/kg/min (max 5 mcg/kg/min) [4].
Nitroglycerin and sodium nitroprusside (Nipruss®) provide NO•. Nitogylcerin preferentially vasodilates the great central veins (capacitance vessels) while sodium nitroprusside's action is chiefly focused on the resistance vessels. Only nitroglycerin is used as a pulmonary vasodilator, since sodium nitroprusside leads to excessive systemic hypotension. Dosage: 0.5-5.0 mcg/kg/min.
Pulmonary vasodilatators
Pulmonary vasodilators include inhaled agents (NO, prostaglandins, milrinone), intravenous substances (prostaglandins, milrinone, sildenafil) and oral medications used in chronic treatment (see Table 14.7 and Paediatric Pulmonary Hypertension) [1].
NO is indicated for persistent pulmonary hypertension in neonates and also for numerous paediatric congenital heart diseases, extending into the postoperative phase following cardiac surgery (RV failure, heart transplant, Fontan physiology, etc.). Dosage: 10-20 ppm in the inspiratory circuit. Side effects: methaemoglobinaemia, NO2 formation, platelet aggregation inhibition, rebound effect on treatment discontinuation.
Sildenafil is a phosphodiesterase-5 inhibitor, which is available in intravenous form. Although the IV form has not been officially approved, it is increasingly used in three scenarios: preventing postoperative PAH crises, treating right-side failure, and discontinuing NO [1]. Dosage: 0.35 mg/kg over 20 minutes, repeated 3 times per day.
Prostaglandins act by stimulating adenylyl cyclase, increase cAMP levels, and prompt quite selective vasodilation of the pulmonary system. They are inhaled or administered intravenously as a chronic or acute treatment and exhibit an additive effect with NO• in reducing PVR in cases of PAH and lowering RV afterload [7,9].
- Iloprost (Ilomedin®) as a nasal spray (2.5-5.0 mcg in 15 min 6-8 x/d) or nebulised;
- Epoprostenol (Flolan®) as a continuous infusion (5-15 ng/kg/min) by central line;
- Treprostinil administered sub-cutaneously (1.25-2.5 ng/kg/min).
Prostaglandin E1 (Prostin VR®) is no longer used due to its side effects. It is currently only used to keep the ductus arteriosus open in neonatal heart diseases that are dependent on it (TGA, interrupted aortic arch, etc.). Prostaglandins inhibit platelet adhesiveness.
| Perioperative haemodynamic drug therapy |
|
There are three objectives for drug therapy provided to patients with congenital heart diseases:
- Optimise O2 delivery and cardiac output - Maintain organ perfusion pressure - Maintain an optimal balance between pulmonary and systemic blood flow (Qp/Qs = 1) The preferred inotropic agent is a combination of epinephrin + milrinone. |
© BETTEX D, BOEGLI Y, CHASSOT PG, June 2008, last update February 2020
References
- AVILA-ALVAREZ A, DEL CERRO MARIN MJ, BAUTISTA-HERNANDEZ V. Pulmonary vasodilators in the management of low cardiac output syndrome after pediatric cardiac surgery. Curr Vascul Pharmaco 2016; 14:37-47
- CHANG A, ATZ A, WERNOVSKY G, et al. Milrinone: Systemic and pulmonary hemodynamic effects in neonates after cardiac surgery. Crit Care Med 1995; 23:1907-14
- MAHAJAN A, MARIJIC J. Hemodynamic management. In: ANDROPOULOS DA, et al, eds. Anesthesia for congenital heart disease. Oxford: Blackwell-Futura, 2005, 225-40
- OLIVEIRA NICOLAU G, NIGRO NETO C, LUCENA BEZERRA FJ, et al. Vasodilator agents in pediatric cardiac surgery with cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2018; 32: 412-22
- PISANO A, MONTI G, LANDONI G. Levosimendan: new indications and evidence for reduction in perioperative mortality ? Curr Opin Anaesthesiol 2016; 29:454-61
- POLLESELLO P, PARISSIS J, KIVIKKO M, et al. Levosimendan meta-analyses: is there a pattern in the effect on mortality ? Int J Cardiol 2016; 209: 77-83
- RICH S, MCLAUGHLIN VV. The effects of chronic prostacyclin therapy on cardiac output and symptoms in primary pulomonary hypertension. J Am Coll Cardiol 1999; 34:1184-7
- ROSENZWEIG E, STARC T, CHEN J, et al. Intravenous argini-vasopressin in children with vasodilatory shock after cardiac surgery. Circulation 1999; 100:182-6
- SCHROEDER RA, WOOD GL, PLOTKIN JS, et al. Intraoperative use of inhaled PGI(2) for acute pulmonary hypertension and right ventricular failure. Anesth Analg 2000; 91:291-5
- STOCKER CF, SHEKERDEMIAN LS, NORGAARD MA, et al. Mechanisms of a reduced cardiac output and the effects of milrinone and levosimendan in a model of infant cardiopulmonary bypass. Crit Care Med 2007; 35:252-9
- TOLLER W, ALGOTSSON L, GUARRACINO F, et al. Perioperative use of levosimendan: best practice in operative settings. J Cardiothorac Vasc Anesth 2013; 27:362-6
- TWEDDELL J, HOFFMAN G, FEDDERLY R, et al. Phenoxybenzamine improves systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg 1999; 67:161-7
